Prevention and preparedness to health threats pose several challenges: to identify multifactorial drivers, to detect and evaluate risks as early as possible, to involve multiple actors and stakeholders, and to make information and data transversely and transparently accessible.
This requires a coordinated, multidisciplinary and multisectoral effort by the systems involved, which presently communicate with difficulty in a fragmented context.
One Health can provide strategic scientific support if governance, research and training aim to overcome the barriers that hamper interaction, collaboration and coordination between sectors and disciplines.
We call on the G20 to lead concrete actions that are capable of transforming the current One Health momentum into long-term commitments.
Challenge
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), responsible for the COVID-19 pandemic, emerged and rapidly spread around the world with a devastating death toll (almost 4 million victims at mid-June 2021) and a predicted global economic loss set at over €18 trillion between 2020 and 2025 (IMF, 2021).
The COVID-19 pandemic showed that while global health threats may be triggered by individual agents, the scenario that emerges is necessarily one that involves a multitude of factors (such as socio-economic, cultural and environmental) that affect communities on a global scale, well beyond the specific biological effects of an individual agent. For this reason, the impact can be said to be “syndemic”; that is, determined by aggregated or synergistic interactions with other adverse health, socio-economic and environmental conditions.
At the same time, it is misleading to trace any pandemic to a single trigger without considering the multifarious causes, complex determinants and drivers that contributed to its occurrence.
Unfortunately, to date, health systems have operated in isolation, and global preparedness (in the form of collection and translation of knowledge, training of personnel, procedures and plans required in the event of a health emergency) has been sought without involving all the relevant disciplines and stakeholders.
This hampers evaluation of the possible consequences and unequal impacts of the pandemic on countries, communities and various sectors of society.
In addition, the prevailing approach to epidemics and pandemics attempts merely to control health hazards once they emerge (or re-emerge). An efficient global preparedness strategy should instead promptly assess the multiple potential risk factors that are involved before they become a threat, so as to prevent or mitigate their consequences.
The zoonotic origin of most emerging pathogens, the crucial role played by humans in the over-exploitation of the environment and the complexity of socio-economic drivers involved in the emergence and spread of epidemics requires a holistic One Health approach, which should be designed and implemented in order to improve the effectiveness of prevention and preparedness plans.
One Health represents a valid scientific strategy, but its adoption in plans and policies both at governmental and international level requires aspects of governance, research and training to be addressed, so that the current fragmentation and barriers (including silos in education and siloed funding) can be overcome, as these hamper the interaction, collaboration and coordination between sectors and disciplines that are required.
At present, stand-alone national One Health plans are often developed. However, in order to benefit from this approach, efforts should be made to appropriately integrate One Health strategies into relevant national and international plans.
It is therefore necessary to develop adequate frameworks and to identify procedures that allow this integration, together with effective implementation of comprehensive prevention and preparedness strategies.
Proposal
RATIONALE FOR ENHANCING PREVENTION AND PREPAREDNESS PLANS WITH ONE HEALTH STRATEGIES
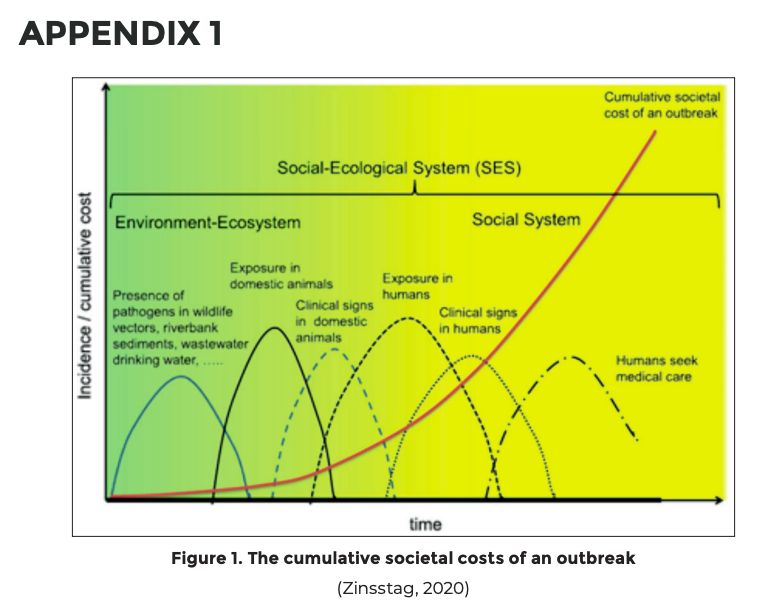
The need to prevent and early detect to reduce the societal costs of a pandemic
The cumulative societal costs of an outbreak were highlighted for the first time by the World Bank (World Bank, 2012) and then discussed by experts in emerging infectious diseases (IDs) (Zinsstag, 2020). The moment in which a system is able to detect signals of possible threats was correlated with the possible costs for the system. That is, the earlier the detection of these signals, the lower the costs for the systems involved (Fig. 1 in Appendix 1).
The impacts on the systems that are called to respond to any epidemics vary in accordance with their local fragilities (e.g. availability of services, economic development, poverty, social inequity, health coverage, presence of other epidemics, societal turmoil and wars). Therefore, the impact on services and related health and socio-economic repercussions should be evaluated according to context (Economist at Large, 2011; Gongal, 2020).
A recent review on the long-term societal impacts of COVID-19 outlined a series of important social, economic and cultural effects on three main areas of society: health and well-being (including physical and mental health and the environment); communities, culture and belonging; and knowledge, employment and skills (British Academy, 2021). It has been reported that the pandemic highlighted and also significantly worsened social inequalities, with dramatic consequences for vulnerable groups (Tsai, 2020; Solis, 2021).
The Intergovernmental Science-Policy Platform on Biodiversity and Ecosystem Services Workshop Report on Biodiversity and Pandemics (2020) provides numerous evidence-based actions that could start a paradigm shift: “The current pandemic preparedness strategy involves responding to a pandemic after it has emerged. Yet, the research reviewed in this report identifies substantial knowledge that provides a pathway to predicting and preventing pandemics. This includes work that predicts geographic origins of future pandemics, identifies key reservoir hosts and the pathogens most likely to emerge, and demonstrates how environmental and socioeconomic changes correlate with disease emergence” (IPBES, 2020).
The need to consider integrated drivers for epidemic/pandemic preparedness
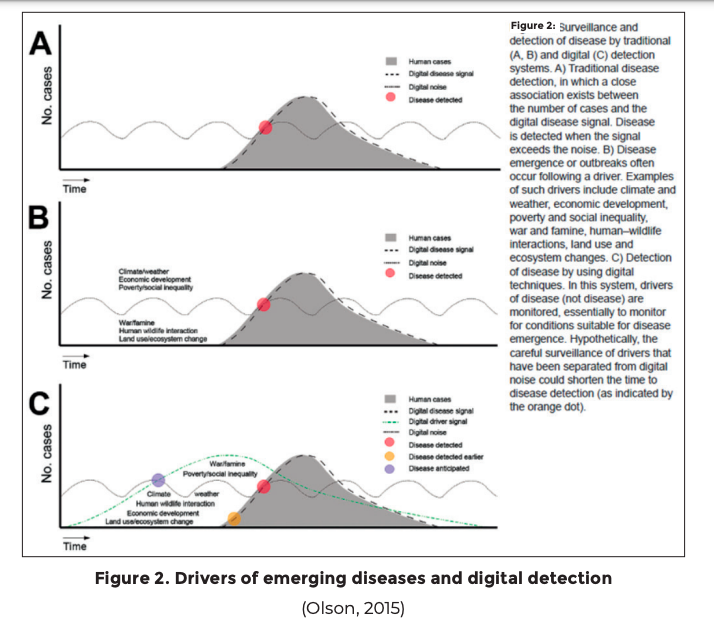
Many of the upstream drivers of disease occur outside the human health sector (e.g. animal health, land use, loss of biodiversity, urbanization, conflicts and climate change), and are multifactorial.1 Understanding and addressing them requires greater attention to be placed on the prevention and detection of threats, ideally before they cause disease outbreaks. Effectively addressing these drivers brings in a wider range of potential partners, including government, society and the private sector, which can combine resources, strategies and solutions to create better global and local public health policies.
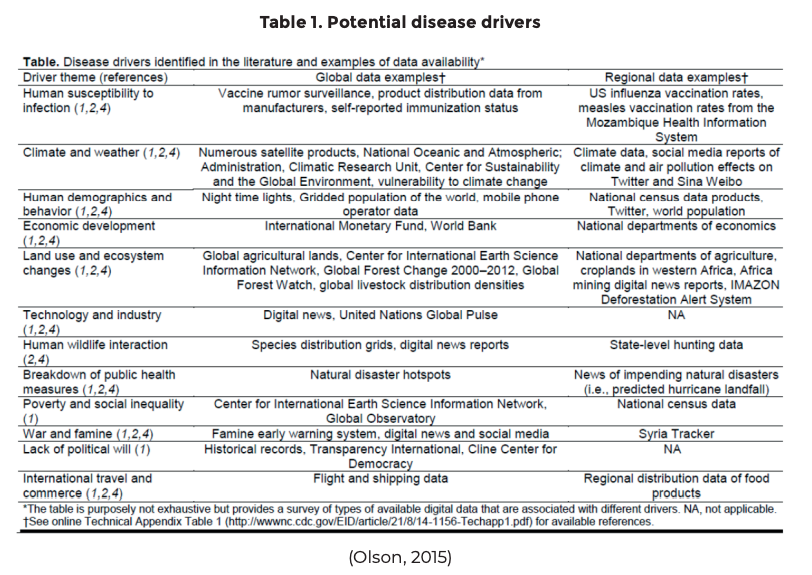
Behind the development of surveillance tools for ID events, growing research suggests that untapped driver signals could be quantified and monitored to anticipate emergence risk as a new form of epidemic intelligence. Temperature and precipitation data are already used to forecast meteorologically sensitive IDs, but more driver data could support improved predictive models covering a much broader range of health threats. Logically, further strengthening of public health could take place through the expansion of surveillance, so that the full spectrum of ID emergence drivers are monitored (Fig. 2 and Table 1 in Appendix 1) (Olson et al., 2015).
The mainstreaming of disease prevention into national plans for climate adaptation, biodiversity, environmental protection and other sectors can help to reduce risks upstream and promote early warning for disease threats (Machalaba et al., 2018).
The need to consider the multiplicity of the actors, stakeholders, disciplines and related interests involved in prevention and preparedness measures
There are many intervention areas that should consider the multiplicity of the factors involved. Emblematic of these is the example of the implementation of biosecurity measures in live animal markets, intensively farmed chickens and pigs, and in other interfaces between animals (wildlife and domestic species). Drastic measures (e.g. the closing of markets, an increase in the spacing between animals on farms) can lead to a loss of income, and to poverty and hunger for large numbers of small-scale famers. There are also ethical and cultural issues that need to be considered (Zahouli et al., 2017).
For this reason, all stakeholders (e.g. farmers, traders, butchers, consumers, communities, administrators and scientists) should be involved to identify locally adapted biosecurity and animal welfare measures, while maintaining economic activity. To prevent future pandemics, there is a pressing need to deepen the understanding of pathogen transmission between the environment, wildlife, domestic animals and humans as part of a complex social and ecological system (Zinsstag, 2020).
The potential social and economic impact, and related ethical aspects, should also be carefully considered when formulating policies that are aimed at protecting the environment and its biodiversity. For example, it is instructive to understand how to counter the correlation that has emerged between vector-borne and zoonotic disease outbreaks and changes in forest cover and oil palm expansion. With an increase in plantation monocultures, which has decreased afforestation, an increase in epidemics of zoonotic diseases has been recorded, as well as an increase in the transmission of IDs by insects (Morand and Lajaunie, 2021).
This is likely to take place because that some species act as a filter to diseases and guarantee a natural regulation of diseases, which is lost as biodiversity decreases. As the protection of global biodiversity is instrumental in preventing the emergence of future pandemics, deforestation should be stopped as soon as possible.
In this case, it is necessary to consider how to operate at various levels. Impositions from above are unlikely to succeed, with effective compliance being better achieved through participative involvement. For this reason, ethical issues are very significant: farmers who lose their income when changing crops ought to be compensated or helped to convert their activities. More generally, the potential health problems related to their activities and the overall well-being of those involved ought to be considered (Morand et al., 2021). The same applies to the regulation of wet markets and other economic activities or traditions that have not only an economic but also a cultural value (Zahouli et al., 2017).
Community engagement is the other critical aspect to consider when enhancing preparedness to potential threats (WHO, 2020b) and ensuring a rapid response aimed at reducing rather than exacerbating social and health inequities (Alberti, Lantz and Wilkins, 2020).
In order to build trust and empower multiple stakeholders, countries must prioritize a locally tailored One Health approach to community engagement. Communities’ involvement and an appropriate risk communication strategy can substantially mitigate an outbreak’s severity as well as enhance communities’ long-term resilience (Dickmann et al., 2018).
Investing and actively promoting “whole of society” approaches,2 in order to ensure preparedness strategies and capabilities that detect, respond to and mitigate the effects of emergent health threats across the entirety of society by establishing and strengthening relationships between health and non-health sectors is pivotal (Machalaba et al., 2018).
The more all the sectors involved collaborate to deploy an integrated prevention and preparedness strategy, the more the cumulative societal costs of a possible pandemic can be reduced.
The need to promptly access and share information and data transparently
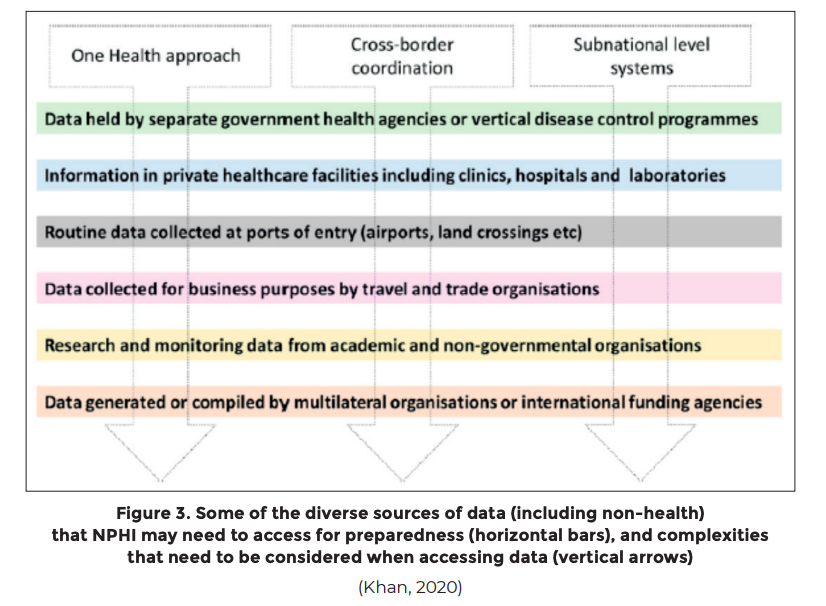
Effective access to, and use of, data from National Public Health Institutes (NPHIs) or their equivalent is a critical building block of national preparedness. To enhance NPHI functioning, it is essential that they routinely access and monitor a broad set of priority indicators that are selected to reflect the country-specific context (Fig. 3 in Appendix 1) (Khan et al., 2020).
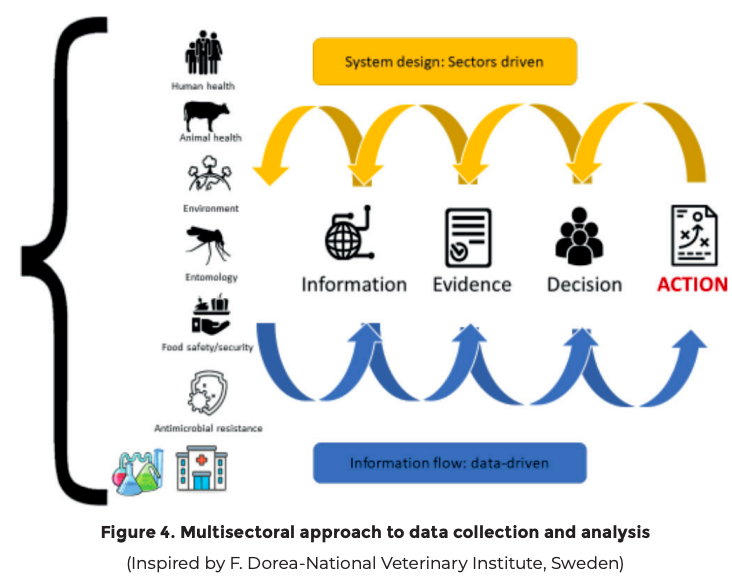
As the COVID-19 pandemic has shown, information and data collected by all the relevant sectors/stakeholders, both public and private, should be made available to allow multisectoral analysis and provide evidence for appropriate decisions and related actions (Naguib et al., 2020).
Education plays a decisive role in training a new generation of policymakers, scientists, public managers and community leaders capable of promoting and making operational a multidisciplinary and multisectoral approach that makes possible data sharing and coordinated analysis through knowledge, innovation and international academic collaboration (Chan and Fu-Chun, 2021).
OPERATIONALIZATION OF ONE HEALTH
Considering the challenges we have discussed, the implementation of One Health strategies represents added value both for prevention and preparedness.
One Health deals with complex health issues and addresses risk factors and threats at the human-animal-environment interface, thereby enhancing and contributing to preparedness capacity.
Prevention strategies based on One Health principles raise awareness that protection of ecosystem balance and biodiversity are priority actions to reduce the risk of pandemics. Through the integration of data from various disciplines, One Health encourages coordination, collaboration and communication among the social and the biomedical sciences, while promoting integrated (ethically and epistemically sound) public health policies.
The adoption of One Health strategies can help to reduce the risks of potential epidemics (prevent), support the early identification of epidemic risks (alert); contribute to the reduction of the impact of potential epidemics/pandemics (mitigate).
In recent years, and even more so in light of the consequences of the COVID-19 pandemic, there have been many international calls and initiatives that have been advocating for a global paradigm shift based on One Health (Richardson et al., 2016; WHO, FAO, OIE, 2019; European Commission, 2020; IPEBS, 2020; Bronzwaer et al., 2021; Gruetzmacher et al., 2021), and the One Health approach is now often advocated by national pandemic plans.
On 16 March 2021, the Pan-European Commission on Health and Sustainable Development (Pan-European Commission on Health and Sustainable Development, 2021) called on governments, economic and social stakeholders, and international organizations to rethink their broad policy priorities, to step up investment in and reforms of health and social care systems, and to upgrade the global governance of public goods, such as health and the environment. The One Health approach is the fulcrum of all the identified priorities. It facilitates full, universal and sustained compliance with the World Health Organization (WHO) International Health Regulations (IHR-2005) and adopts strategies and approaches that recognize multisectoral responses are vital (Machalaba, 2018).
The G20 Health Working Group, the Global Health Summit 2021, the G20 Rome Declaration and finally the Carbis Bay G7 Summit 2021 have raised awareness of One Health preparedness, recognizing that (re) emerging of threats to health are caused by a disequilibrium at the human-animal-environment interface.3 In such a context, we should promptly address those organizational, ethical, educational, resource and epistemic aspects that reduce the operationalization of One Health at national and international level (Landford, 2012; Marcotty et al., 2013; Connolly, 2017; Berthe et al., 2018; Johnson et al., 2018; van Herten et al., 2019; Dos S Ribeiro et al., 2019; etc.).
RECOMMENDATIONS FOR THE G20
With this momentum apparent, the G20 should play a leading role in overcoming the barriers and the lukewarm global engagement and commitment that are still hampering One Health’s contribution to prevention and preparedness policies. We therefore put forward the following recommendations for consideration:
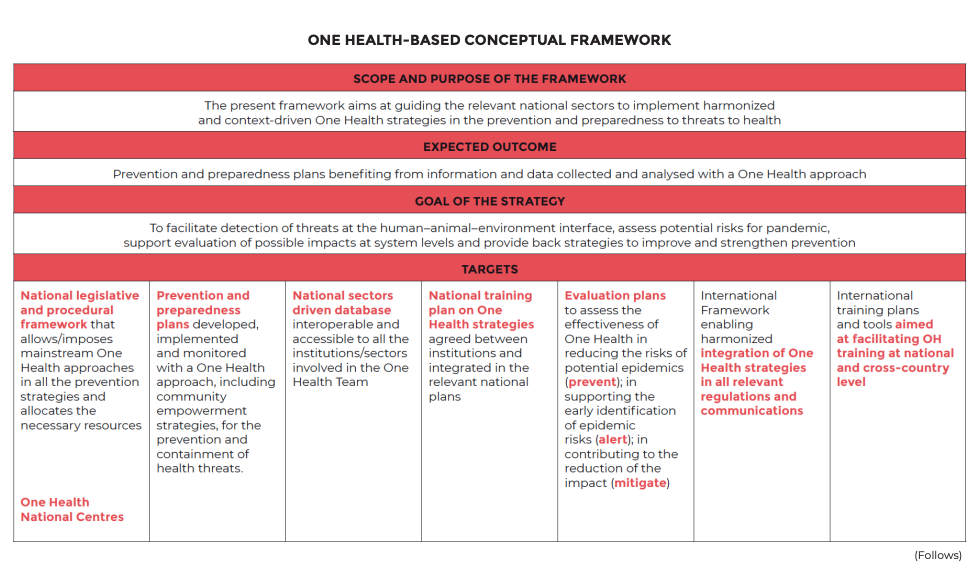
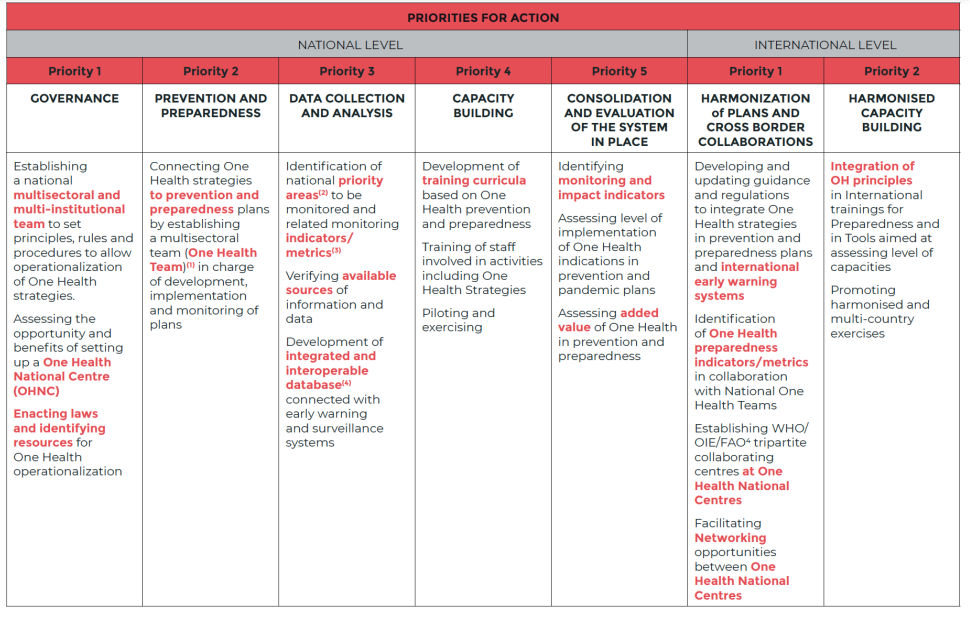
– Promoting the adoption of a One Health-Based Conceptual Framework for operationalization at national level: a strategy to promote the use of One Health approaches in prevention and preparedness is the implementation of a One Healthbased Conceptual Framework (OHCF) that ensures the adoption of comprehensive risk analysis and preparedness plans and their harmonization with identified priorities for action. The OHCF is a multidisciplinary effort aimed at prevention, identification of risks for pandemics and the related possible impacts on society. The information and data collected, analysed with a One Health approach, support the elaboration and updating of prevention and preparedness plans and provide evidence for appropriate decisions and related actions (Appendix 2).
– Governance: mandating to relevant international bodies the formulation of guidance and related enforcement mechanisms for a specific governance structure across sectors and disciplines at national and international level, to ensure harmonized institutionalization of One Health strategies (including guidance for setting means for integrated data collection and analysis, risk assessment, resource allocation, after action reviews and training). Lessons learned from individual countries should be considered in relation to different contexts of implementation such as in the establishment of One Health centres, a One Health directorate and a One Health national steering committee.
– Integration of One Health strategies in all relevant national and international plans: mandating to international relevant bodies the formulation of guidance and related enforcement mechanisms to integrate One Health strategies in all relevant prevention and preparedness plans developed at national level and in all relevant international regulations and communications as well as in related simulation exercises. Moreover, a locally tailored One Health strategy for community and civil society engagement through awareness and effective risk communication should be included in the integrated plans.
– Integrated risk assessments: building international guidance and tools to integrate One Health risk assessment of relevant threats at national and subnational level. This approach should mediate between approaches that already exist and new forms of risk assessment in different sectors, thus capitalizing on the strengths of tested methodologies.
– Cost-effectiveness evaluation: mandating to international relevant bodies the development, in coordination with the countries that are already implementing One Health strategies, of a harmonized cost-effectiveness evaluation framework, with modular options to tailor for local conditions, including ad hoc operational research, to assess and quantify the added value of One Health strategies in the fields of prevention and preparedness.
– Training and capacity building: promoting and supporting, with adequate resources at national level, the integration of One Heath strategies in relevant curricula, and facilitating the development of a common culture of preparedness. This includes the capacity to design and conduct integrated One Health simulation exercises and advance knowledge sharing and capacity building in all priority technical sectors (e.g. data collection, sharing and analysis; communication, modelling, after action evaluation, joint risk assessment and One Health preparedness planning).
Accordingly, we suggest that the G20 should include the following wording in its final communiqué:
Promote the adoption of a One Health-Based Conceptual Framework for integration of One Health in prevention and preparedness at national level.
International relevant bodies, in coordination with the governments implementing One Health Strategies, should provide guidance and related enforcement mechanisms for:
– a specific One Health governance structure across sectors and disciplines, and for integration of One Health in all relevant national and international plans;
– conducting integrated One Health risk assessment of relevant threats at national and subnational level; and
– a harmonized cost-effectiveness evaluation framework, with modular options to tailor for local conditions, including ad hoc operational research, to assess and quantify the added value of One Health strategies in the fields of prevention and preparedness.
Promote and support with adequate resources at national level the integration of One Health strategies in relevant curricula and facilitate the development of a common culture of preparedness.
Progress towards these priorities will be discussed at the G20 2022.
APPENDIX 1
APPENDIX 2
THE ONE HEALTH-BASED CONCEPTUAL FRAMEWORK
A strategy to promote the use of a OH approach in prevention and preparedness is the development of a One Health-Based Conceptual Framework (OHCF) to ensure comprehensiveness in risk analysis, preparedness plans and their harmonization.
The OHCF is a multidisciplinary effort aimed at prevention, identification of risks for pandemics and related impacts on society.
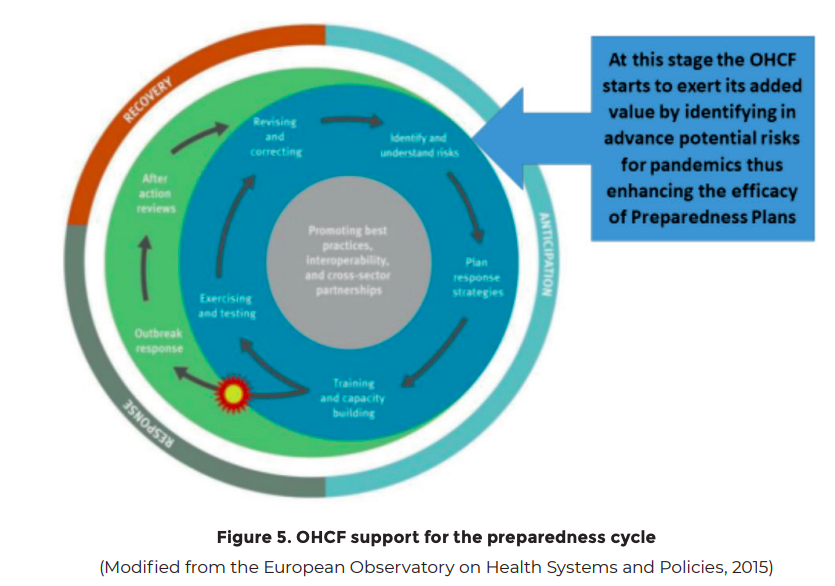
The information and data collected, analysed with a One Health approach, support the elaboration and updating of prevention and preparedness plans and provide evidence for the appropriate decisions and related actions (Fig.5).
One Health applies to all related actions, including the identification of priorities through the systematic collection and interpretation of integrated data, multisectoral capacity building and risk assessment, and the regular update and monitoring of existing plans across sectors.
The risk indicators should be applicable worldwide, with options to tailor to local conditions, and they should be assessed and analysed at country level to highlight prevailing vulnerabilities. Risk indicators include aspects related to potential health threats identified at the human-animal-environment interface, as well as key fragilities of national systems (health, social, economic, etc.).
The risk analysis will also provide information that helps to improve prevention plans and actions in a continuum of processes fed and supported by the OHCF (Fig. 6).
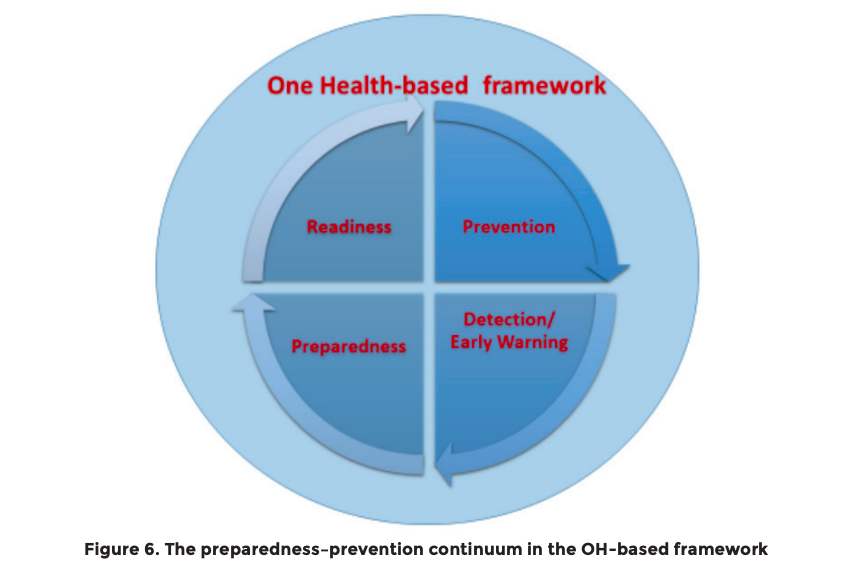
Taking into consideration other frameworks that have been developed for other purposes but with similar comprehensive strategies (UNISDR, 2015; WHO, 2016, 2020; Machalaba, 2018; Alberti, 2020) and more specific One Health frameworks (Dente et al., 2018; ECDC, 2018, 2021; Machalaba, 2018; Farag, 2019; Pelican et al., 2019; WHO, FAO, OIE, 2019; Africa CDC, 2020; Amato, 2020; FAO, 2020), the following One Health-Based Conceptual Framework is proposed.
It aims to support the detection of threats at the human-animal-environment interface, assessing potential risks for pandemics, evaluating possible impacts at system levels and providing back strategies to improve and strengthen prevention.
It addresses priorities for action to be considered at national (by governments) and international (by international organizations and agencies) level.
Some countries might have already started One Health operationalization, and therefore some priorities might have been already accomplished. Each country will implement the OHCF in accordance with local situations and contexts.
The establishment of One Health National Centres (OHNCs) is a strategic opportunity to facilitate the national coordination of all the sectors/stakeholders/institutions involved and consistency in the identification of priorities for research and action. This will facilitate governance and efficient utilization of available resources.
International institutions will have the main role of facilitating the networking of OHNCs and supporting the harmonization of procedures and trainings by formulating guidance and related enforcement mechanisms.
Framework notes
(1) The One Health team may be or may be not the one that has developed the governance
(National Institutional Team). In fact, One Health strategies can benefit several sectors and domains, so an appropriate institutional team should develop a governance that considers all the stakeholders involved. For the sake of this framework, the One Health team should include all the competencies and disciplines relevant for prevention and preparedness purposes.
(2) Priority areas refer to areas that may be at risk of favouring the development of epidemic events (Zahouli et al., 2017; Nuzzo et al., 2019; Meyer et al., 2020; Ministero della Salute, 2021; Plowright et al., 2021)
Therefore, in this context, a priority area might be:
– a vast market zone trading in wild animals;
– an area with migration movements/camps;
– an area subjected to intense climatic variations and/or manmade exploitation;
– an ecosystem particularly stressed favouring spillover events;
– populations professionally exposed to possible transitions of species;
– a fragile area in terms of low level of health coverage, low preparedness capacity, missing data collection and sharing.
(3) Indicators/metrics should consider what has already been developed and implemented in the context of relevant surveillance/early warning/preparedness national and international systems and the priority area/s identified.
(4) The integrated and interoperable database should consider relevant platforms developed/being developed at national and international level (e.g. VEO, 2021)
NOTES
1 The concept of drivers is used in different fields, including economics, social sciences, technology, health and environmental sciences. Drivers are defined as issues that shape the development of a society, organization, industry, research area, technology, etc. They may act as facilitators or modifiers of effect on the onset of emerging risks. Namely, drivers can either amplify or attenuate the magnitude or frequency of risks arising from various sources (Richardson et al., 2016).
2 Whole of government and whole of society approaches are grounded in strategies that enhance joined-up government, improved coordination and the integration and diffusion of responsibility for health throughout government and society. Health is an emerging property of many societal systems; therefore it requires action in many systems, sometimes with and sometimes without the involvement of the health sector (WHO Regional Office for Europe, 2011).
3 Carbis Bay G7 Summit Communiqué, 13 June 2021 Statements and Releases “Improving integration, by strengthening a ‘One Health’ approach across all aspects of pandemic prevention and preparedness, recognising the critical links between human and animal health and the environment”: https://www.whitehouse.gov/briefing-room/statements-releases/2021/06/13/ carbis-bay-g7-summit-communique/?mc_cid=0a36c74d2b&mc_eid=UNIQID.
4 WHO: World Health Organisation; OIE: World Organisation for Animal Health; FAO: The Food and Agriculture Organization.
REFERENCES
Africa CDC and Africa Union (2020). Framework for One Health Practice in National Public Health Institutes. Zoonotic Disease Prevention and Control
Alberti PM, Lantz PM, Wilkins CH (2020). Equitable pandemic preparedness and rapid response: lessons from COVID-19 for pandemic health equity. Journal of Health Politics, Policy and Law, 45(6):921-935, https://doi.org/10.1215/03616878-8641469, accessed 12 July 2021
Amato L, et al. (2020). Integrated early warning surveillance: Achilles’ heel of One Health? Microorganisms, 8(1):84, https://doi.org/10.3390/microorganisms8010084, accessed 12 July 2021
Berthe FCJ, et al. (2018). Operational Framework for Strengthening Human, Animal and Environmental Public Health Systems at their Interface. Washington, DC: World Bank Group, https://documents.worldbank.org/curated/en/703711517234
British Academy (2021). The COVID Dec ade: Understanding the Long-Term Societal Impacts of COVID-19. London: British Academy, https://www.thebritishacademy.ac.uk/publications/covid-decade-understanding-the-long-term-societal-impacts-of-covid-19/, accessed 12 July 2021
Bronzwaer S, et al. (2021). Editorial: EFSA’s expertise supports One Health policy needs. EFSA Journal, 19(5):e190501, https://doi.org/10.2903/j.efsa.2021.e190501, accessed 12 July 2021
Carroll D, et al. (2018). The Global Virome Project. Science, 359(6378): 872-874, https://dx.doi.org/10.1126/science.aap7463, accessed 12 July 2021
Chan Fung, MF (2021). Overcoming complacency in the face of infectious disease. Nature Medicine, 27(363), https://doi.org/10.1038/s41591-021-01259-z, accessed 12 July 2021
Connolly J (2017). Governing towards “One Health”: establishing knowledge integration in global health security governance. Global Policy, 8(4):483-494. doi:10.1111/17585899.12505
Dente MG et al. (2018). Strengthening preparedness for arbovirus infections in Mediterranean and Black Sea countries: a conceptual framework to assess integrated surveillance in the context of the One Health strategy. International Journal of Environmental Research and Public Health, 15(3):489, https://doi.org/10.3390/ijerph15030489, accessed 12 July 2021
Dickmann P, et al. (2018). Kampala manifesto: building community-based One Health approaches to disease surveillance and response-the Ebola legacy-lessons from a peer-led capacity-building initiative. PLOS Neglected Tropical Diseases, 12(4):e0006292, https://doi.org/10.1371/journal.pntd.0006292, accessed 12 July 2021
Dobson A, et al. (2020). Ecology and economics for pandemic prevention. Science, 369(6502):379-381, https://science.sciencemag.org/content/369/6502/379/tab-pdf, accessed 12 July 2021
Dos S Ribeiro C, et al. (2019). Overcoming challenges for designing and implementing the One Health approach: a systematic review of the literature. One Health (Amsterdam, Netherlands), 7:100085. doi: 10.1016/j.onehlt.2019.100085
ECDC (European Centre for Disease Prevention and Control) (2018). Towards One Health Preparedness. Stockholm: ECDC, https://www.ecdc.europa.eu/sites/default/files/documents/One-Health-preparedness-24-May-2018.pdf, accessed 12 July 2021
ECDC (European Centre for Disease Prevention and Control) (2021). Assessment Tool for Joint “One-Health” Country Visits in Relation to Antimicrobial Resistance. Stockholm: ECDC, https://www.ecdc.europa.eu/sites/default/files/documents/One-Health-AMR-assessment-tool-forcountry-visits.pdf, accessed 12 July 2021
Economists at Large, Campbell R, Knowles T (2011). The Economic Impacts of Losing Livestock in a Disaster. Melbourne: WSPA, https://www.gndr.org/images/newsite/Learning/Animal-Protection/EcolargeLivestockDisasterEconomics-Final.pdf, accessed 12 July 2021
European Commission (2020). Communication from the Commission to the European Parliament, the Council, the European Economic and Social Committee and the Committee of the Regions Building a European Health Union: Reinforcing the EU’s Resilience for Cross-Border Health Threats. Brussels: European Commission, https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=CELEX%3A52020DC0724, accessed 12 July 2021
European Observatory on Health Systems and Policies et al. (2015). Enhancing public health preparedness: towards an integrated process. Eurohealth, 21(3):36-39, https://apps.who.int/iris/handle/10665/332756, accessed 12 July 2021
FAO (Food and Agricultural Organization of the United Nations) (2020). Preventing the next zoonotic pandemic: Strengthening and extending the One Health approach to avert pandemics of animal origin in the region. Budapest: FAO, https://doi.org/10.4060/cb2017en, accessed 12 July 2021
Farag EAB, et al. (2019). Survey on implementation of One Health approach for MERS-CoV preparedness and control in Gulf Cooperation Council and Middle East countries. Emerging Infectious Diseases, 25, https://doi.org/10.3201/eid2503.171702, accessed 12 July 2021
Gongal G, Ofrin, RH (2020). Animal welfare, One Health and emergency preparedness and response in the Asia-Pacific region. WHO South-East Asia Journal of Public Health, 9:50-51, https://doi.org/10.4103/2224-3151.282996, accessed 12 July 2021
Gruetzmacher K, et al. (2021). The Berlin principles on One Health: bridging global health and conservation. Science of the Total Environment, 764:142919, https://doi.org/10.1016/j.scitotenv.2020.142919, accessed 12 July 2021
IMF (International Monetary Fund), et al. (2021). Transcript of the World Economic Outlook update press briefing, Washington, 28 January, https://www.imf.org/en/News/Articles/2021/01/28/tr012621-transcript-of-the-world-economic-outlook-update-press-briefing, accessed 12 July 2021
IPBES (Intergovernmental Science-Policy Platform on Biodiversity and Ecosystem Services), et al. (2020). Workshop Report on Biodiversity and Pandemics. Bonn: IPBES, https://doi.org/10.5281/zenodo.4147317, accessed 12 July 2021
Johnson I, et al. (2018). The challenges of implementing an integrated One Health surveillance system in Australia. Zoonoses and Public Health, 65(1):e229-e236. doi:10.1111/zph.12433
Khan MS, et al. (2020). Using critical information to strengthen pandemic preparedness: the role of national public health agencies. BMJ Global Health, 5(9), https://doi.org/10.1136/bmjgh-2020-002830, accessed 12 July 2021
Landford J (2012). Good governance in “One Health” approaches. Revue Scientifique et Technique de l’OIE, 31(2):561-575
Machalaba CC, et al. (2018). Institutionalizing One Health: from assessment to action. Health Security, 16, https://doi.org/10.1089/hs.2018.0064, accessed 12 July 2021
Marcotty T, et al. (2013). Intersectoral collaboration between the medical and veterinary professions in low-resource societies: the role of research and training institutions. Comparative Immunology, Microbiology and Infectious Diseases, 36(3):233-239
Meyer D, et al. (2020). A checklist to improve health system resilience to infectious disease outbreaks and natural hazards. BMJ Global Health, 5(8), https://dx.doi.org/10.1136/bmjgh-2020-002429, accessed 12 July 2021
Ministero della Salute (2021). Piano strategico-operativo nazionale di preparazione e risposta a una pandemia influenzale (Pan Flu) 2021-2023, Gazzetta Ufficiale Serie Generale 23. Rome: Ministero della Salute, https://www.salute.gov.it/portale/nuovocoronavirus/dettaglioPubblicazioniNuovoCoronavirus.jsp?id=3005, accessed 12 July 2021
Morand S, Lajaunie C (2021). Outbreaks of vector-borne and zoonotic diseases are associated with changes in forest cover and oil palm expansion at global scale. Frontiers in Veterinary Science, 8, https://doi.org/10.3389/fvets.2021.661063, accessed 12 July 2021
Naguib MM, et al. (2020). Towards pandemic preparedness beyond COVID-19. The Lancet Microbe, 1(5):E185-E186, https://doi.org/10.1016/s2666-5247(20)30088-4, accessed 12 July 2021
Nuzzo JB, et al. (2019). What makes health systems resilient against infectious disease outbreaks and natural hazards? Results from a scoping review. BMC Public Health, 19(1):1310, https://doi.org/10.1186/s12889-019-7707-z, accessed 12 July 2021
Olson SH, et al. (2015). Drivers of emerging infectious disease events as a framework for digital detection. Emerging Infectious Diseases, 21(8), https://doi.org/10.3201/eid2108.141156, accessed 12 July 2021
Pan-European Commission on Health and Sustainable Development (2021). Rethinking Policy Priorities in the Light of Pandemics: A Call to Action. Copenhagen: Pan-European Commission, https://www.euro.who.int/__data/assets/pdf_file/0010/495856/Pan-European-Commission-Call-to-action-eng.pdf, accessed 12 July 2021
Pelican K, et al. (2019). Synergising tools for capacity assessment and One Health operationalisation. Revue Scientifique et Technique de l’OIE, 38(1):71-89, https://dx.doi.org/10.20506/rst.38.1.2942, accessed 12 July 2021
Plowright RK, et al. (2021). Land use-induced spillover: a call to action to safeguard environmental, animal, and human health. Lancet Planet Health, 5(4):e237-e245, https://doi.org/10.1016/S2542-5196(21)00031-0, accessed 12 July 2021.
Richardson J, et al. (2016). Drivers for emerging issues in animal and plant health. EFSA Journal, 14(S1), https://doi.org/10.2903/j.efsa.2016.s0512, accessed 12 July 2021
Solis A, Nunn CL (2021). One Health disparities and COVID-19. Evolution, Medicine, and Public Health, 9(1):70-77, https://doi.org/10.1093/emph/eoab003, accessed 12 July 2021
Tsai J, Wilson M (2020). COVID-19: a potential public health problem for homeless 414 populations. The Lancet Public Health, 5(4):e186-187, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7104053/pdf/main.pdf, accessed 12 July 2021
World Bank (2012). People, Pathogens and our Planet: Volume 2: The Economics of One Health (Report no. 69145-GLB). Washington, DC: World Bank, https://openknowledge.worldbank.org/handle/10986/11892, accessed 12 July 2021
UNISDR (United Nations Office for Disaster Risk Reduction) (2015). Sendai Framework for Disaster Risk Reduction 2015-2030. Geneva: UN, https://www.unisdr.org/files/43291_sendaiframeworkfordrren.pdf, accessed 12 July 2021
van Herten J, et al. (2019). One Health as a moral dilemma: towards a socially responsible zoonotic disease control. Zoonoses and Public Health, 66(1):26-34. doi:10.1111/zph.12536
VEO (Versatile Emerging Infectious Disease Observatory) (2021). Project: early detection of infectious disease, Cordis, https://cordis.europa.eu/project/id/874735/it, accessed 12 July 2021
WHO (World Health Organization) Regional Office for Europe (2011). Governance for Health in the 21st Century. Baku: WHO, https://www.euro.who.int/__data/assets/pdf_file/0019/154252/Health-2020-Conf.Governance-for-health-…pdf, accessed 12 July 2021
WHO (World Health Organization) (2016). Tool for Influenza Pandemic Risk Assessment. Geneva: WHO, https://www.who.int/influenza/publications/TIPRA_Guidance_version_2.pdf?ua=1, accessed 12 July 2021
WHO (World Health Organization) (2020a). Quality of Care in Fragile, Conflict-Affected and Vulnerable Settings: Taking Action. Geneva, WHO, https://www.who.int/publications/i/item/9789240015203, accessed 12 July 2021
WHO (World Health Organization) (2020b). A World in Disorder: Global Preparedness Monitoring Board Annual Report. Geneva: WHO, https://apps.who.int/gpmb/assets/annual_report/2020/GPMB_2020_AR_EN_WEB.pdf, accessed 12 July 2021
WHO, FAO, OIE (World Health Organization, Food and Agriculture Organization, World Organisation for Animal Health) (2019). Taking a Multisectoral, One Health Approach: A Tripartite Guide to Addressing Zoonotic Diseases in Countries. Geneva: WHO, https://www.who.int/publications/i/item/taking-a-multisectoral-one-health-approach-a-tripartite-guide-to-addressing-zoonotic-diseases-in-countries, accessed 12 July 2021
Zahouli JBZ, et al. (2017). Effect of land use changes on the abundance, distribution, and host-seeking behavior of Aedes arbovirus vectors in oil palm-dominated landscapes, southeastern Côte d’Ivoire. PLOS ONE, 12, https://doi.org/10.1371/journal.pone.0189082, accessed 12 July 2021
Zinsstag J, et al. (2020). Towards integrated surveillance-response systems for the prevention of future pandemics. Infectious Diseases of Poverty, 9:140, https://doi.org/10.1186/s40249-020-00757-5, accessed 12 July 2021