COVID-19 has had an unprecedented impact on global health but the inequitable consequences have been as expected. As the pandemic has exploited and exacerbated pre-existing disparities within and between countries, it has led to a renewed focus on the meaning of global health equity. The intersection between the harm caused by the virus and the reverberations associated with acute social disruption and the probable long-term consequences for learning, health, health systems resilience, equity and economic prosperity require us to reconsider how we define and value global health in the wake of the pandemic.
Challenge
Global health equity is discussed in different contexts relating to development: as a policy goal, a field of research, an ethical imperative, a health sciences discipline and as the overarching theme of a university (Drobac and Morse, 2016). However, in order to understand what global health equity might truly mean, particularly through the lens of the recent pandemic, it is worth revisiting each concept that is encompassed by this term.
GLOBAL
Global perspectives require a lens through which the outcomes for all are equally valued, regardless of national borders, gender, age, race or ethnicity, ability or income. At its core, a global lens requires us to assess needs and priorities at supranational level. This is akin to conceptualizing the earth as a single country in which all citizens are viewed as having the same fundamental rights, such as the right to health (OHCHR, 2021). Beyond this, however, there is an acknowledgement of global interconnectedness. COVID-19 has demonstrated the extent to which global health is a social good, a necessary foundation for global prosperity (Abdalla et al., 2020).
HEALTH
The World Health Organization (WHO, 1948) defines health as “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity”. This definition has historically been criticized on philosophical grounds as being overly broad and moving beyond a purely medical focus (Callahan, 1973). With the passage of time, however, the value in this definition has come to be understood, as physical and mental health are to a large degree a function of our physical and social environments (Marmot et al., 2008). As the COVID-19 pandemic has shown, social divides determine our health outcomes to a large degree and are as deadly as any external pathogen (Bambra et al., 2020; Maani and Galea, 2020). It has also shown the extent to which conditions and activities outside hospitals and clinics, in the home, at work or in school, that ultimately determine our health status as individuals and communities. Health, then, is about much more than healthcare, as it also reflects the upstream distribution of opportunity and resources.
EQUITY
Equity describes the just and fair allocation of resources according to need. It describes the absence of avoidable differences among groups, whether we define these by their geographic location, rurality, economic status or social standing. In the context of health, it refers to the allocation of resources according to need, in such a way that preventable differences in health outcomes are minimized and access is fair (Culyer and Wagstaff, 1993). However, in being reminded of the broader drivers of health that are articulated in the WHO definition of health, it becomes clear that equity in the context of health requires equity in the political, social and economic conditions that generate health. For this reason, it has been argued that global health is not merely an academic discipline, but “a collection of problems [that] … turn on the quest for equity” (Farmer et al., 2013). In this sense, equity is also a foundation for prosperity and resilience, allowing a greater number of people a greater degree of autonomy and resources with which to respond to new economic opportunities and overcome unexpected shocks, such as COVID-19.
Proposal
EQUITABLE DISTRIBUTION OF HEALTH BETWEEN AND WITHIN COUNTRIES
Before the pandemic, significant gaps remained in life expectancy between countries, even though there has been a rapid narrowing of global gaps in the last fifty years (Roser, Ortiz-Ospina and Ritchie, 2013). There are many reasons for this. While medical innovation has played a role, particularly in the context of vaccine distribution, at the global level improvements in population health been largely due to improvements in living conditions, employment and education associated with economic development. Significant health inequalities between countries remain, and while income inequality in relative terms is decreasing between countries, the gap in absolute mean per capita incomes in low and high income countries continues to grow (UN DESA, 2020). COVID-19 and its economic and social consequences, which include an estimated additional 119-24 million people pushed into extreme poverty (Lanker et al., 2021), and more generally trends in greater unemployment and poorer education outcomes among lower-income workers (ILO, 2021), risk worsening health gaps between countries long into the future.
Beyond life expectancy, disease burden is also inequitably distributed. When examining disability adjusted life years, a measure of disease burden expressed as the number of years of life lost to disability, ill health, or early death, the WHO’s Africa region continues to experience a disproportionately high disease burden (see Figure 1), primarily driven by neonatal conditions and preventable infectious diseases such as lower respiratory infections, malaria, diarrhoeal diseases, HIV/AIDS and tuberculosis. Achieving global health equity would mean a world in which this disproportionate and avoidable disease burden, which primarily affects the very young and the very poor, would be eliminated.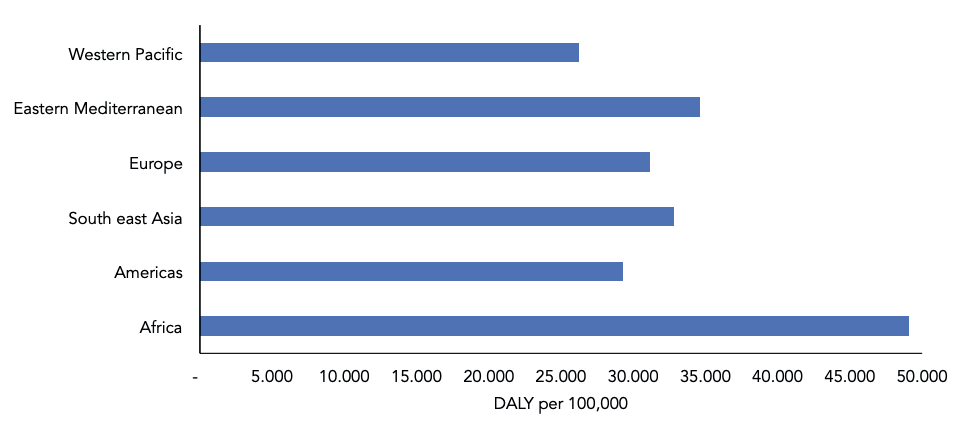
Figure 1. Disability-adjusted life years per 100,000 population by region
Source: Adapted from the World Health Organization Global Health Observatory (WHO-GHO, 2021). Global Health Estimates: Life expectancy and leading causes of death and disability: World Health Organization, https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates
However, just as global improvements in health have been driven by reductions in poverty and improvements in living standards, a substantial resource disparity between the Global North and Global South represents a political and economic power imbalance that risks obstructing multilateralism and the protection and growth of global public goods (Abdalla et al., 2020). Pre-COVID-19, this manifested in many ways, including trade objections by high-income countries that prevented national public health regulations in lowand middle-income countries (Barlow et al., 2018; Barlow and Stuckler, 2021), and during the pandemic, the stockpiling of vaccine and personal protective equipment by high-income countries at the expense of lowand middle-income countries (Wouters et al., 2021). In other words, between-country health inequalities during COVID-19 were in part a consequence of between-country power and resource inequalities that already existed.
A WORLD WHERE HEALTH IS NOT INEQUITABLY DISTRIBUTED WITHIN COUNTRIES
Taking a truly global view of health equity requires us to consider the inequitable distribution of health not only across countries, but also within countries, regions, cities and neighbourhoods. Being female, higher income, and more educated are associated with greater longevity across the distribution curve around the world, but within-country gaps in health and life expectancy can differ significantly. For example, in the United States in 2016, men aged 40 in the highest 1 per cent of earners had an expected age of death of 87.3 years, 14.6 years longer than those in the bottom 1 per cent of earners. The equivalent gap for women was 10.1 years (Chetty et al., 2016). Taking full definitions of health and well-being beyond longevity, being female is associated with greater exposure to mental illness and gender-based violence (WHO, 2021).
There are also urban-rural divides. For example, life expectancy at birth in India is 71.6 years in the wealthiest quintile of men, decreasing to 63.2 in the poorest quintile overall, but these gaps are larger in urban households (9.1 years) than in rural households (7.5 years) (Asaria et al., 2019). More broadly, regional differences reflecting resource and opportunity gaps can lead to significant within-country variance. In the United Kingdom, life expectancy in the most deprived regions in 2013 was comparable to the life expectancy in 1990 for least deprived regions (Newton et al., 2015). This means that even in high-income countries, there are significant proportions of the population that are “left behind”, experiencing shorter lives in poorer health than the wealthiest minorities in many lowand middle-income countries, often along racial and ethnic divides (Wrigley-Field, 2020). By contrast, wealthy minorities in many lowand middle-income countries, particularly in Latin America, Africa and east Asia, make a much greater proportion of overall national income. In other words, income inequality is more extreme. It is clear then that both between and within-country inequities are obstacles to global health equity. Both had roles to play in ill health before the pandemic, and both have been exacerbated by COVID-19.
It is important, however, to understand differences in within and between-country health inequalities, as their causes, measurement and solutions vary, and there may be trade-offs when focusing on one factor or another. For example, trade agreements that widen access to the global economy may reduce between-country health inequalities, but prove a catalyst for the widening of health inequalities within a country if the benefits disproportionately fall to a wealthier and more educated subsection of the population, while the risks, in the form of job loss, outsourcing or reduced employment rights, fall disproportionately on less skilled workers (UNCTAD, 2019).
Persistent within-country inequalities in high-income settings may also undermine public support for investment in overseas development. Understanding and mitigating these trade-offs is critical as both between and within-country health gaps pose threats to global health equity and global prosperity. When considering between-country or within-country differences, it is clear that health inequities arise owing to wider inequalities in the allocation of power, resources and opportunity, and it is through this lens that we must examine and overcome barriers to global health equity.
WHAT HAS INHIBITED GLOBAL HEALTH EQUITY?
Three main areas have inhibited progress towards global health equity.
A narrow emphasis on what shapes health, available to a few
In contrast with our broad definition of global health equity, global health research in practice reflects a narrow emphasis on particular health outcomes in particular settings. A recent meta-knowledge analysis found that global health research tended to focus on infectious diseases in lowand middle-income settings and on healthcare systems (Abdalla et al., 2020). Current global health research is predominantly focused on biomedical and healthcare solutions to diseases that are unique to low-income settings (Abdalla et al., 2020), rather than focusing on the reasons why these diseases continue to challenge lowand middle-income countries, or taking a wider and truly global view (consistent with how the field is defined in theory) and concentrating on global challenges such as urbanization, climate change, antimicrobial resistance and income inequality (Abdalla et al., 2020).
A lack of focus on the foundational causes of health, which are highly inequitable in their distribution
A focus on the downstream and biomedical solutions to global health equity has also led to a lack of focus on the social determinants of health, the physical and social environments in which we live, even though these are highly inequitable in their distribution and contribute disproportionately to health inequity within and between countries. Indeed, it was a focus on the more downstream and biomedical definitions of health that contributed to the assumption that high-income countries would be resilient to a potential pandemic in the years prior to COVID-19. In reality, upstream factors such as a lack of investment in wider social protections and widening socio-economic divides along racial and ethnic divides, together with the longer term defunding of public health infrastructure, greatly undermined the response to the pandemic in countries such as the United States and worsened its impact (Bambra et al., 2020; Maani and Galea, 2020).
Research across a range of lowand middle-income countries has shown the extent to which these long-standing divides pose more than merely technocratic, quantitative challenges to healthcare access. They are accompanied by differences in soft power and prestige, supported by long-standing values and norms. These can contribute to feelings of stigma, marginalization, dispossession and diminishment when engaging with authorities, including health authorities, and this exacerbates divides in health and human capital (Morgan et al., 2018; de França, Modena and Confalonieri, 2020). This means that some groups, already in poorer health and less able to weather unexpected crises, may fear engagement with authorities or health providers in the context of testing or vaccination. COVID-19 has demonstrated that no amount of biomedical capacity can overcome these societal failures. This is also true for health outcomes more generally.
A lack of focus on the causes of inequitable distributions
Failing to understand the causes of health has led to a lack of focus on the upstream power and economic imbalances that prevent a more equitable distribution of resources; this is necessary to reduce global health inequity. Without addressing this issue, the response to the COVID-19 pandemic will fail to improve the underlying health divides that COVID-19 has exploited, and the adaptability and resilience of the global population to future health challenges will not be enhanced.
TOWARDS GLOBAL HEALTH EQUITY
Vision
As made evident in this brief, achieving true global health equity requires a real engagement with the achievable but specific health inequity challenges we face within and between countries. It also requires engagement with the broader, deeper power and economic inequities that ultimately underpin these challenges. This requires us to consider global values that can guide international and national levels of action alike, as both are fundamental components of global health equity. We should also consider all outcomes in terms of health equity, since health is affected by decisions across government departments (HiAP, 2014). We can think of a technical solution for a single dimension of health equity in a single context, or we can grapple with international and intranational equity priorities. While it is harder politically to tackle broader capacity building and development, and to reduce inequity of resources, opportunities and power, this is a practical and moral imperative in the longer term.
Proceeding in this manner will challenge our emphasis on voluntary agreements for initiatives such as COVAX, as donors have a strong preference for downstream and specifically measurable outcomes rather than broader, longer-term investments in areas such as education, housing, energy, and infrastructure that to a great degree ultimately influence global health equity.
Finally, we should consider the immediate challenges that health inequities pose, and also the long-tail consequences of our decisions to reduce global health inequities over the longer term.
BOX 1
Values that Could Guide Global Equity Priorities – Equity is a critical component of resilience and disease prevention.
– Reducing health inequity necessitates that we reduce underlying inequities, rather than just extremes of poverty.
– This includes both withinand between-country inequities.
– All decisions that affect equity affect health.
– The urgency of the moment must be balanced with addressing the causes of the moment.
Recommendations
1. Develop truly global metrics of health inequity
In a globalized era, health equity both within and between countries is a foundational pillar of global prosperity. Understanding health inequities is therefore key to preparing for future pandemics. Current metrics of health inequalities focus primarily on healthcare-related outcomes, rather than encompassing the foundational drivers of ill health. We propose the development of global metrics of health inequity, emerging from the broadest definition of health and linking to the social determinants of health. This will allow funders, non-governmental organizations and governments a clearer view of the longer-term projections for health inequity, their implications for policy, health and prosperity, and the likely impact of future shocks and changes in policy.
2. Develop a forum for global health equity
In order to best understand critical vulnerabilities, and to track progress made in addressing health inequities within and between countries, we propose the establishment of a global health equity forum that combines data on within-country and between-country health inequity, and the underlying drivers of this inequity. Such a forum could leverage existing health data collection innovations and data on key pillars of health equity such as education, employment and infrastructure, and also identify critical data gaps. In doing so, it could observe critical health equity goals, identify examples of best practice applicable in different contexts and predict critical health equity challenges. In addition to the practical value of this, the forum could also serve to increase global solidarity by identifying the common health challenges linked to inequity that are faced by groups across different national contexts.
In the context of a future pandemic, each of these components would identify critical “weak links” in the global population that involve a lack of access to social protections, labour standards, public health and healthcare services. A forum could help to predict those subpopulations within countries that are most likely to require additional support in times of natural or manmade disasters, and identify groups that are likely to be disproportionately affected by global policy goals, such as reducing CO2 emissions.
3. Document inequities across and within countries that were present before COVID-19 and those that have been widened as a result of the COVID-19 pandemic
It is imperative that one of the first tasks for such a forum would be developing metrics that can adequately catalogue and seek to rectify inequalities that have arisen as a result of COVID-19. Recent world events have shown the extent to which lingering economic inequality and stagnation following the global financial crisis (2007-8) provided tinder, in the form of a lack of trust in institutions and the media, divestment of social goods and an increase in those “left behind”, all of which made for combustible political and economic developments. COVID-19 has both exploited and exacerbated such divides with devastating health consequences, laying bare pre-existing social divides in the form of differences in COVID-19 exposure, infection and death rates, and in the differing abilities to weather physical distancing measures by working and learning remotely. A failure to document these divides would have negative consequences for health equity, and could also adversely affect future resilience, political stability and public trust in decision-making. This is of particular note at a time when decision-makers are grappling with global measures such as those aimed at lowering emissions.
4. Develop systems of global accountability for health equity
Data on the root causes of global health inequity will be insufficient without complementary systems of global accountability. According to the WHO, transformational accountability in the context of health equity “would need to expose the structural barriers (the social, economic and political structures, policies and mechanisms that shape the unfair and inequitable distribution of, and access to, power, wealth and other resources) and commercial determinants that are barriers to health equity” (Hammonds, Hanefeld and Ooms, 2019).
Adopting purely voluntary and state-led measures in the context of inequity is challenging because of the context-specific nature and often deep-seated cultural origins of such inequities. In order for countries, non-governmental agencies and funders to be held to account on the need for investment in foundational drivers of health equity rather than continuing to focus exclusively on downstream biomedical interventions, it is critical that systems of accountability that include local stakeholders are built, and that periodic reporting to mechanisms such as United Nations Special Rapporteurs and committees is guaranteed.
APPENDIX
ADDRESSING GLOBAL HEALTH EQUITY: EXAMPLES OF DOWNSTREAM AND UPSTREAM CHALLENGES DURING COVID-19
DOWNSTREAM CHALLENGE: COVID VACCINE ALLOCATION
One of the most prominent examples of a barrier to global health equity has been the misallocation of COVID-19 vaccines within and between countries. In spite of the development of the COVID-19 Vaccines Global Access Facility (COVAX), which encourages high-income nations to guarantee equitable access to these vaccines worldwide, high-income countries have reached bilateral agreements with manufacturers for a large proportion of available doses. By February 2021, while high-income countries represent only 16 per cent of the global population, they had purchased approximately 50 per cent of all COVID-19 vaccine doses, enough to vaccinate their populations more than twice over (Rouw, 2021; Yamey, 2021). But over 100 countries had yet to administer a single vaccine dose. Globally, those in greatest need of vaccines are those most vulnerable to the virus (the elderly and those with health conditions that place them at greater risk of severe illness) and those most exposed to the virus (healthcare and other essential workers), irrespective of their country of residence. Failing to take a global approach is resulting in the prolongation of the pandemic and the likely exacerbation of socio-economic divides between countries.
This focus on allocation between countries should not distract from the inequity in vaccination within countries, which is also a pressing concern owing to urban-rural divides and to racial, ethnic, tribal and class differences in health status, ability to access healthcare and exposure to the virus owing to housing, employment or educational conditions. Vaccination rates within countries may also vary depending on the levels of trust in institutions and historical experience with them. This means the relationship between equity and vaccine distribution is dynamic, and builds on previous actual and perceived treatment of different groups.
Therefore, at the root of health inequity in the context of vaccine distribution, both between and within countries, is an underlying inequity in resources, opportunity and power. While a fuller embrace of COVAX, or more equitable guidelines for the distribution of vaccines within countries, might reduce health inequities in the context of COVID-19, the conditions that drive those health inequities in the first place, the vast differences in underlying health status, access to healthcare, infrastructure for storing and transporting medicines, access to safe working and housing conditions, and imbalances in ability to influence trade agreements or patent protections would remain. It is therefore imperative to consider fundamental inequities in power and resources as well as short-term solutions to improve equity to vaccine access.
UPSTREAM CHALLENGE: ECONOMIC CONSEQUENCES OF THE COVID-19 PANDEMIC
The COVID-19 pandemic has led to global reverberations far beyond the millions of lives lost or altered as a direct result of infection. These include the economic consequences of the pandemic and the measures taken to restrict its spread. The implementation of social distancing itself is likely to have significant repercussions for global health equity, owing to the consequences of economic shutdown that are being faced by vulnerable or marginalized groups.
The ability to work remotely is a privilege that is afforded to a minority of the global population, as is the guarantee of a continued salary during the implementation of movement restriction measures. Globally, COVID-19-related unemployment and income losses have affected women, younger workers, the self-employed and lowand medium-skilled workers the most (ILO, 2021). School closures disproportionately affect the most vulnerable children, such as those in foster care or with special educational needs, and place additional burdens on parents who cannot work remotely, as well as households without internet and computing equipment, space to study or available adult supervision (Nicola et al., 2020; Viner et al., 2021). By some estimates, as many as 11 million girls may not return to education, instead facing an increased risk of early forced marriage, adolescent pregnancy or violence (UNESCO, 2021). These are disparities that have both immediate and long-tail consequences.
Such gaps in education or employment risk future gaps in attainment and assets, which will then lead to widening gaps in health inequalities in the years and decades ahead. Again, this vulnerability to the longer-term consequences of the pandemic is a manifestation of inequity in terms of living conditions, resources and rights that predated the pandemic, as is the case for inequities in vaccine distribution.
REFERENCES
Abdalla SM, et al. (2020a). Claiming health as a public good in the post-COVID-19 era. Development, 63(2):200-204. doi: 10.1057/ s41301-020-00255-z
Abdalla SM, et al. (2020b). What is considered as global health scholarship? A meta-knowledge analysis of global health journals and definitions. BMJ Global Health, 5(10):e002884. doi: 10.1136/bmjgh-2020-002884
Asaria M, et al. (2019). Socioeconomic inequality in life expectancy in India. BMJ Global Health, 4(3):e001445. doi: 10.1136/ bmjgh-2019-001445
Bambra C, et al. (2020). The COVID-19 pandemic and health inequalities. Journal of Epidemiology and Community Health, 74(11):964-968. doi: 10.1136/jech2020-214401
Barlow P, et al. (2018). Trade challenges at the World Trade Organization to national noncommunicable disease prevention policies: a thematic document analysis of trade and health policy space. PLoS Med, 15(6):e1002590. doi: 10.1371/journal. pmed.1002590
Barlow P, Stuckler D. (2021). Globalization and health policy space: introducing the WTOhealth dataset of trade challenges to national health regulations at World Trade Organization, 1995-2016. Social Science & Medicine, 275:113807, https://doi.org/10.1016/j.socscimed.2021.113807, accessed 12 July 2021
Callahan D. (1973). The WHO definition of “health”. The Hastings Center Studies, 1(3):77-87. doi: 10.2307/3527467
Chetty R, et al. (2016). The association between income and life expectancy in the
United States, 2001-2014. JAMA, 315(16):17501766. doi: 10.1001/jama.2016.4226
Culyer AJ, Wagstaff A. (1993). Equity and equality in health and health care. Journal of Health Economics, 12(4):431-457, https://doi.org/10.1016/0167-6296(93)90004-X, accessed 12 July 2021
de França VH, Modena CM, Confalonieri UEC. (2020). Equality and poverty: views from managers and professionals from public services and household heads in the Belo Horizonte Metropolitan Area, Brazil. International Journal for Equity in Health, 19(1):132. doi: 10.1186/s12939-02001243-y
Drobac P, Morse M. (2016). Medical education and global health equity. AMA Journal of Ethics, 18(7):702-709. doi: 10.1001/ journalofethics.2016.18.7.medu1-1607
Farmer P, et al. (2013). Reimagining Global Health: An Introduction. Berkeley: University of California Press
Hammonds R, Hanefeld J, Ooms G (2019). Accountability as a Driver of Health Equity. Copenhagen: World Health Organization Regional Office for Europe
HiAP (Health in All Policies) (2014). Health in All Policies (HiAP) framework for country action. Health Promotion International, 29 Suppl 1:i19-28, https://doi.org/10.1093/heapro/dau035, accessed 12 July 2021
ILO (International Labour Organization) (2021). ILO Monitor: COVID-19 and the World of Work. 7th edition. Cham, Switzerland: International Labour Organization
Lanker C, et al. (2021). Updated Estimates of the Impact of COVID-19 on Global Poverty: Looking Back at 2020 and the Outlook for 2021. World Bank Blogs. Washington, DC: World Bank
Maani N, Galea S (2020). COVID-19 and underinvestment in the health of the US population. Milbank Quarterly, 98(2):239-249, https://doi.org/10.1111/14680009.12462, accessed 12 July 2021
Marmot M, et al. (2008). Closing the gap in a generation: health equity through action on the social determinants of health. The Lancet, 372(9650):1661-1669
Morgan R, et al. (2018). Gendered health systems: evidence from low- and middle-income countries. Health Research Policy and Systems, 16(1):58. doi: 10.1186/ s12961-018-0338-5
Newton JN, et al. (2015). Changes in health in England, with analysis by English regions and areas of deprivation, 1990&2013: a systematic analysis for the Global Burden of Disease Study 2013. The Lancet, 386(10010):2257-2274. doi: 10.1016/ S0140-6736(15)00195-6
Nicola M, et al. (2020). The socio-economic implications of the coronavirus and COVID-19 pandemic: a review. International Journal of Surgery, 78:185-193, https://doi.org/10.1016/j.ijsu.2020.04.018, accessed 12 July 2021
OHCHR (Office of the UN High Commissioner for Human Rights) (2021). OHCHR and the right to health: United Nations, https://www.ohchr.org/EN/Issues/ESCR/Pages/Health.aspx, accessed 12 July 2021
Roser M, Ortiz-Ospina E, Ritchie H (2013). Life expectancy. OurWorldInData, https://ourworldindata.org/life-expectancy, accessed 1 April 2021
Rouw A, et al. (2021). Global COVID-19 vaccine access: a snapshot of inequality.
Kaiser Family Foundation, https://www.kff.org/policy-watch/global-covid-19-vaccine-access-snapshot-of-inequality/, accessed 12 July 2021
UNCTAD (United Nations Conference on Trade and Development Secretariat) (2019). Trade Policies and their Impact on Inequalities. Geneva: United Nations
UN DESA (United Nations Department of Economic and Social Affairs) (2020). World Social Report 2020: Inequality in a Rapidly Changing World. Geneva: United Nations
UNESCO (United Nations Educational Scientific and Cultural Organization) (2021). Keeping girls in the picture. UNESCO, https://en.unesco.org/covid19/educationresponse/girlseducation, accessed 22 April 2021
Viner R, et al. (2021). Impacts of school closures on physical and mental health of children and young people: a systematic review. medRxiv, 12 February, https://doi.org/10.1101/2021.02.10.21251526, accessed 12 July 2021
WHO (World Health Organization) (1948). Constitution of the World Health Organization. Geneva
WHO (World Health Organization) (2021a). Mental health and substance abuse, https://www.who.int/teams/mental-health-andsubstance-use/gender-and-women-smental-health, accessed 19 April 2021
WHO (World Health Organization) (2021b). Violence against women, https://www.who.int/news-room/fact-sheets/detail/violence-against-women, accessed 19 April 2021
WHO-GHO (World Health Organization Global Health Observatory) (2021). Global health estimates: life expectancy and leading causes of death and disability, https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates, accessed 1 April 2021
Wouters OJ, et al. (2021). Challenges in ensuring global access to COVID-19 vaccines: production, affordability, allocation, and deployment. The Lancet, 397(10278):10231234. doi: 10.1016/S0140-6736(21)00306-8
Wrigley-Field E. (2020). US racial inequality may be as deadly as COVID-19. Proceedings of the National Academy of Sciences of the United States of America, 117(36):2185421856. doi: 10.1073/pnas.2014750117
Yamey G. (2021). Rich countries should tithe their vaccines. Nature, 590(7847):529