Challenge
Proposal
More people live longer – but with more diseases
During the 20th century, the world population increased from an estimated 1.65 billion to 6 billion (United Nations Secretariate, 1999), it will reach 8.6 billion in 2030 and 11.2 billion in 2100 (United Nations, 2017). In recent years, fertility rates have declined in almost all regions of the world, leading to slower growth, but at the same time to an ageing population. The Global Burden of Disease Study 2016 shows that people live longer, but with more diseases. As the global burden of disease is shifting from infectious diseases to non-communicable diseases, chronic conditions such as diabetes, heart disease and stroke, cancers, mental illness have become the most frequent diseases and the chief causes of death globally. An estimated 72.3% of all deaths in 2016 were from non-communicable diseases. Worldwide deaths from ischemic heart disease have increased by 19% since 2006, deaths from diabetes even by 31% (The Lancet, 2017a). Non-communicable diseases not only represent enormous human suffering, but also astronomic costs.The global economic burden of non-communicable diseases has been estimated at around $47 trillion during 2010 through 2030. (Bloom et at., 2011) This is a challenge for all: science and research, the private sector and industry, civil society and politics.
To reduce the global burden of disease, research and the best of science has to be translated into better health for all. The Sustainable Devolopment Goals (SDG) of the United Nations and the Agenda 2030 provide a comprehensive and a holistic orientation and guideline. This can only be implemented using a trans-sectoral interdisciplinary approach. The concepts of “One Health” and “Planetary Health” are already taking into account the facts, that health of the people can only be achieved, if we include the complex interactions of man with animals and with nature. Animal health and the consequences of environmental factors such as climate changes on health are closely linked.
To be successful, the holistic concept of health as reflected in the SDGs demands a holistic interdisciplinary scientific concept which goes beyond the sucessful, but increasingly specialized understanding and organisaton of conservative school medicine. It is interesting that such a new holistic concept of science has recently emerged. This takes into account the close interactions of human and animal biology, environmental factors such as climate or social determinants as well as behaviour and lifestyle. It is based on the fact that genome sequencing and molecular analysis of the evolution of the life on earth, plants, animals and man provides us with new insights, why our biology is the way it is, why we are frail and why we get sick. This new genomic and molecular understanding of the evolution of man also provides us with new insights how to preseve better health rather than treating desases. The scientific view and new evolutionary understanding of medicine, health and disease takes into account our biology, the environment we live in, and our individual and collective behavior and lifestyles as the decisive and important links between our biology and our environment. Behavior and lifestyles which are not adapted to our biology and the specific environment will lead to incapacitation, disease, failure to reproduce and eventually death. A fish is evolutionary adapted to swim in the water to feed and reproduce otherwise he will not survive.
Analysing our evolutionary biology in combination with the physical, social, economic and cultural facets of our environment and with the behavior and lifestyle-related aspects creates a high level of complexity. This needs to be done, however, if we want to come close to understanding reality and the conditions of our life. The deep understanding of evolution teaches us many lessons. We need to be bold and we have to adopt this new holistic approach to establish a definite crosssectoral thinking for health and disease. We also need to include the experience of different professions with knowledge and experience in biology, medicine, different environments and lifestyles. It thus takes the joint efforts of all stakeholders from science, politics, civil society and the private sector to be able to understand and to be successful in improving health for all. The World Health Summit provides an inclusive international Forum for all partners involved. The best available science and facts have to guide the discussions and the recommendations. There is no alternative for the development of a more holistic approach to health, which includes our biology, the environment and our individual and collective behaviors. This political approach is very convincingly summarized in the Sustainable Development Goals. We need to make their implementation successful. The scientific basis is now available. Global health is a political choice but politics can only be successful if they are based on scientific evidence. All of us need to get involved and we have the responsibility to make the noble goal of health for all a reality.
The sustainable development goals (SDGs)
On 1 January 2016, the 17 Sustainable Development Goals (SDGs) of the 2030 Agenda for Sustainable Development — adopted by world leaders in September 2015 at an historic UN Summit — officially came into force. The UN-led process involved its 193 Member States and global civil society. Over the next fifteen years’ countries will mobilize efforts to end all forms of poverty, fight inequalities and tackle climate change, while ensuring that no one is left behind. The SDGs are also known as Global Goals and build on the success of the Millennium Development Goals (MDGs). The new Goals are unique in that they call for action by all countries, poor, rich and middle-income to promote prosperity while protecting the planet. They recognize that ending poverty must go hand-in-hand with strategies that build economic growth and addresses a range of social needs including education, health, social protection, and job opportunities, while tackling climate change and environmental protection.
While the SDGs are not legally binding, governments are expected to take ownership and establish national frameworks for the achievement of the 17 Goals. Countries have the primary responsibility for follow-up and review of the progress made in implementing the Goals, which will require quality, accessible and timely data collection. Regional follow-up and review will be based on national-level analyses and contribute to follow-up and review at the global level. All goals are interrelated and are an example of interdisciplinary ambitious policy. Health is affected by and impacts on all other goals as is illustrated below.

Figure 1 SDGs (WHO, www.who.int/sdg/en/)
The SDGs cover a broad range of social and economic development issues and social justice. All goals also relate directly or indirectly to SDG 3: ensure healthy lives and promote wellbeing for all at all ages. Good Health and Well-being for people. This goal replaces several disease specific goals that were part of the Millennium Development Goals (MDGs) which ended in 2015. Unlike the MDGs, the SDG framework does not distinguish between “developed” and “developing” nations, instead, the goals apply to all countries.
Three sectors need to come together in order to achieve sustainable development. These are the economic, social and environmental sectors in their broadest sense. This requires the promotion of multidisciplinary and transdisciplinary research across different sectors, which can be difficult. The SDGs might be contradictory. For example, seeking high levels of global GDP growth might undermine ecological objectives. Yet, more than the MDGs, the SDGs deal with the causes of the problems and try to overcome a silo approach to problems. They also reach out to a plethora of stakeholders including the business community as underlined through Goal 17 on partnerships.
Implementation of the SDGs started worldwide in 2016. This process can also be called “Localizing the SDGs”. All over the planet, individual people, universities, governments and institutions and organizations of all kinds work on several goals at the same time. In each country, governments must translate the goals into national legislation, develop a plan of action, establish budgets and at the same time be open to and actively search for partners. Poor countries need the support of rich countries and coordination at the international level is crucial.
“One Health” and “Planetary Health”: Linking interdependent fields and disciplines within the SDGs
The concept of One Health aims to understand and to improve health and well-being through the prevention of risks and the mitigation of effects of crises that originate at the interface between humans, animals and their various environments. This implies strengthening the collaborative efforts of multiple disciplines. Such an approach is inherently multi-faceted and holistic, and could lead to improvements in alleviating the global burden of disease not only through new advances in drug and vaccine discoveries for human diseases, but also by enabling preventive strategies through insights on plant and animal health and creating health innovation through new knowledge on the interface between humans and their environment.
One Health has not been newly invented. It has been a feature of early approaches to health and medicine since the dawn of civilization, where no major distinction was made between diseases affecting human and animals, and their interplay with their respective ecosystems was always taken into account. Hippocrates’ treatise “On Airs, Waters, and Places” explicitly recognized that the environment was inherently interlinked with health. Such thinking was revived in the 19th century by Rudolf Virchow, who proclaimed that “…between animal and human medicine there are no dividing lines – nor should there be,” which then heralded the advent of the concept of zoonosis and also set the stage for evolutionary medicine to have its future impact.
The strength of One Health, its multi- and interdisciplinary approach, is also its greatest challenge: creating successful collaborations across several disciplines is challenging, as many have not yet recognized their interdependence. Even within the “One Medicine” approach, integrating the fields and stakeholders of the disciplines of anatomy, physiology, biochemistry, genetics, genomics and pathology has proven complicated – let alone their application to both humans and animals and their linkage with environmental factors. The integration of veterinary and human public health perspectives as “One Health” reinforces the interdisciplinary dimension with an intersectoral approach in implementation. Important areas of work are food safety, control of zoonoses such as flu and rabies and the increasing challenge of antimicrobial resistance (AMR).
While the One Health approach has been promoted continuously over the last decades – especially following the Highly Pathogenic Avian Influenza since the end of 2005 – two recent key global health challenges have made it even more relevant: The Ebola outbreak in Western Africa and the urgent need to address AMR before many of the advances of modern medicine are threatened. These two challenges have also highlighted another dimension of One Health – the need to design and implement public health programs that take an integrated approach, as well as the need for policies and regulations that reinforce cooperation and ensure better public health outcomes. This includes multi-sectoral policies and regulatory guidelines concerning poultry and livestock production as well as marketing practices, food safety policies and guidelines, legislation of the use of antibiotics in animals and their enforcement.
At the international level, this has led to increasing collaboration between the World Health Organization (WHO), the Food and Agriculture Organization (FAO) and the Organization for Animal Health (OIE) to protect antibiotics as a global public good. The tripartite cooperation of these three organizations on AMR promotes the prudent and responsible use of antimicrobial agents so that they continue to be effective to treat diseases of public health significance in animals and humans; and to ensure global access to medicines of good quality and fight counterfeit products. In particular, they promote national action plans on AMR which take their starting point from a One Health approach and recognize that AMR does not recognize geographic or human/animal borders.
The Ebola outbreak has highlighted the increasing danger of new emerging infectious diseases that originate in animals and cross over into human populations as ecologic conditions change and many remote areas become more interconnected to the world at large through travel and trade. The response to these new vulnerabilities requires not only medical knowledge and research but also the need to include disciplines such as anthropology and environmental science to understand behaviors such as bush meat hunting and the impact of deforestation on disease and health.
The One Health approach is necessary for all countries, irrespective of their level of development – but holds special significance for least developed countries as 6 out of every 10 infectious diseases in humans are spread from animals. It supports an integrated response to neglected tropical diseases, which affect the poorest countries and populations and works to build and strengthen public health and veterinary health capacity; institutional strengthening and work force development will be key. It is encouraging to see that the One Health approach is becoming an international movement based on transdisciplinarity and cross-sectoral collaboration.
New research frameworks should provide a better understanding of the ecological and environmental factors that impact on human disease to improve preparedness for zoonotic disease outbreaks, emerging infectious diseases in both plants and animals, food safety issues, and antimicrobial resistance.
The need for new scientific holistic concept to improve health globally.
In the past, early diagnosis and efficient treatment of diseases have been in the focus of research and health policy. Education and training of doctors and medical support professions centered on improved treatment of diseases. This is extremely costly and access to medicines is not available in many parts of the world. But health is more than medicine. Evolutionary medicine considers evolutionary theory to explain health and disease. In addition to considering dysfunctions of an organ or a biochemical pathway and trying to interfere in or correct these pathways by chemicals and other interventions, we need to pay more attention to investigating “why” we get sick in the first place. Why is our body the way it is? Why do diseases exist? Why are we frail? Why are diseases of civilization increasing at fast rate? Most importantly: how can we prevent diseases.
Evolutionary medicine can help answer these questions: Advances with new, precise methods in genetics, genome sequencing has enabled us to understand how life developed 3.5 billion years ago and where homo sapiens came from. We know our genes and their history, and we know that the human body is a living archive of evolution. This is one of the important lessons learned and confirmed from the most recent genomic and molecular studies. Darwin’s hypothesis of the origin of species and human evolution has been confirmed by the modern genomic and molecular analysis of all steps of evolution: from bacteria, fish, amphibia, reptiles to mammals, primates and man.
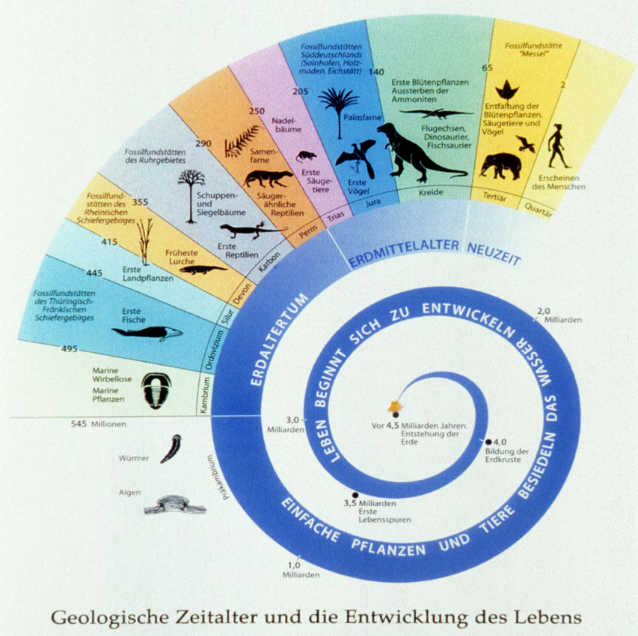
Figure 2 Evolution (Ganten, Nesse 2012)
Evolutionary medicine has thus become a precise and exact new science. We know that we cannot easily get rid of genes and structures once they are part of our genomic heritage. The more important genes are for survival and reproduction, the longer and better they are conserved in evolution. Genes which are important for basic functions are, in general, old genes. Nature is conservative; it conserves structures and genes, rather than function. Gene regulation, cell biology and cell division in humans still follow similar basic mechanism as seen in the first unicellular organisms and in archebacteria as they existed in the beginning of life on earth 3.5 billion years ago. The same is true e.g. for muscles, bones, sensory organs the nervous and the gastro-intestinal systems. The modern human biology is very old and in many instances dates back to the origins of life. The gap between our “old” biology and our modern, fast-changing, frequently man-made new environments explains the diseases of civilization.
An evolutionary perspective of cultures and lifestyles as determinants of health
With our evolutionary ‘old’ biology, we live in a completely new and fast-changing – mostly artificial – man-made environment. The city as an important part of modern human civilisation may serve as an example. Much of modern urbanised society is now dependent on industrially manufactured food, often ordered by smart phone from the department store and delivered home. We eat too much, and consume unhealthy foods that are too salty, too sweet and too fat. (Ganten & Nesse, 2012). This is not limited to industrialized countries: Non-communicable diseases disproportionately affect people in low- and middle-income countries, where more than three quarters of global deaths attributable to NCD – 31 million – occur. (WHO, 2017) These countries thus face a double burden while they undergo the demographic transition of an aging population: as infectious disease rates remain high, non-communicable diseases increase.
Changing living standards in low and middle income countries often go along with changes in lifestyles. Dietary patterns shift from traditional diets low in fat and high in unrefined carbohydrates, to industrially produced and/or imported foods high in fat and salt, and low in carbohydrates, fruit, and vegetables (Chopra et al, 2002). Unhealthy alcohol use and tobacco consumption are the main risk factors for non-communicable disease. Transnational tobacco companies and the alcohol industry have long shifted their marketing to low- and middle income countries, as tobacco and alcohol control activities in the developed world have increased (Beaglehole and Yach, 2003). These industries also increasingly target women, who historically have lower unhealthy drinking and smoking rates, as potential markets to expand to.
Modern medicine and sophisticated methods for the diagnosis, treatment of diseases and prevention of diseases have provided great progress for the health and wellbeing of the people. The access to medicines urgently needs to be improved in many regions of the world so that the people in need can benefit. On the other end of the spectrum, drug abuse and drug dependence, especially with respect to opioids and pain killers, has become a major problem in many societies. Sedentary lifestyles are a major risk factor for non-communicable diseases. Amounts of physical exercise decrease as a result of the urban built environment. In urban settings in Sub-Saharan Africa and elsewhere, public transport replaces the traditional pattern of walking long distances, and urban employment usually entails far less physical labor than rural employment (Steyn & Damasceno, 2006). These entail other risks like indoor pollution, unsafe water and sanitation, and occupational risks.. The gap between evolutionary ‘old’ body functions, on the one hand, and modern lifestyles in new urban societies, on the other, results in cardiovascular diseases, musculo-skeletal dysfunctions, cancer, mental diseases, which make up about 80 percent of the disease burden und health costs. (Ganten & Nesse, 2012). This disease burden is also defined by inequity – in many countries health inequalities have increased.
Health as a cultural, economic and social factor
Health is driven by a combination of biology, environment and behavior, which is determined by a person’s social, cultural, and economic context (cf. figure1).
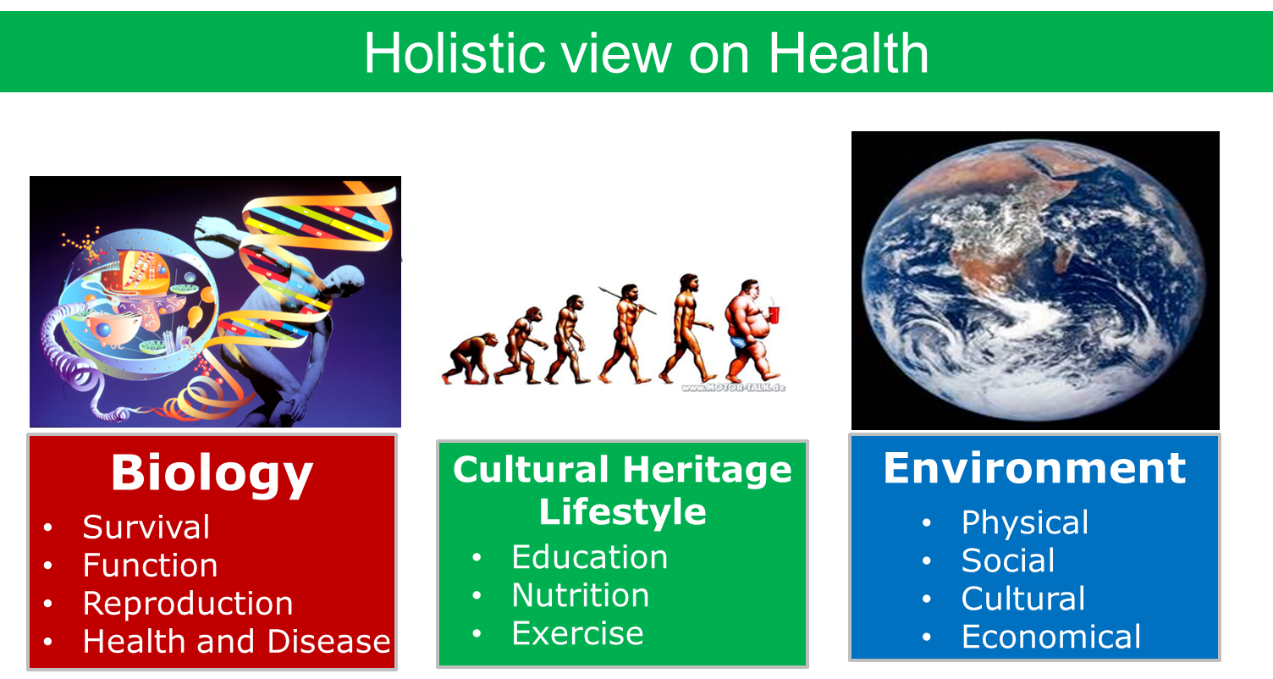
Figure 3: A holistic view of health, based on Ganten & Nesse, 2012).
Many of the non-communicable diseases are promoted by well-identified risk factors, which makes a significant part of them preventable: but they are also related to social and commercial determinants of health. Effective and cost-effective prevention requires collaborative efforts – between politicians, academics, civil society organizations and industry, but also across disciplines and departments.
Health is the largest and most important economic sector, with a unique interdependence between research, innovation and patient care. It includes a range of activities from individual medicine, clinical care to global and public health. In economic terms, the health sector encompasses both services (e.g. hospitals, pharmacies, care facilities, insurance) and industrial manufacturing (e.g. pharma and medtech). It generates gross added value and additionally stimulates growth in many other sectors through complex value chains. Global health expenditures are projected to reach 8.7 trillion USD by 2020, due to improved treatments, rising labor costs and higher life expectancy (Deloitte, 2016).
Citizens across the world are united in citing health as a primary concern (Ipsos Public Affairs, 2017). Good health and wellbeing underpins almost everything that people want – to be free of illness, to escape poverty and hunger, to work to secure independence, to gain fulfilment through education and learning, to be treated fairly and without discrimination, and to live in dignity and in a safe environment. (Dye & Acharya, 2017).
From a societal point of view, investments in health have a huge impact: healthy people implies a healthy workforce. Economic development promotes health, and good population health in turn contributes to further economic development. Several studies have estimated the economic return on investment through different approaches in specific areas such as cardiovascular diseases (Wooding, 2011), cancer (Glover et al., 2014), brain diseases (Sobocki et al., 2006), and musculo-skeletal diseases (Glover et al., 2018).
Scientific progress only reaches a small part of the world’s population
Modern medicine has made great progress: Inventions in basic research, clinical diagnosis and treatment of diseases including scientific microscopy and imaging in conjunction with biochemistry and cell biology laid the foundations for modern pharmacology and therapy in the past century. This is still a basis of medicine as practiced today. Deep sequencing and new technologies in genomics made modern genetics in combination with information technologies, innovations in molecular medicine including single cell sequencing. Analysis of complex interactions at the molecular level are opening up completely new possibilities in understanding human health and disease and innovating therapies and prevention. The progress in sequencing technologies is truly amazing. About fifteen years ago, an international effort to sequence the human genome allowed the first insights into our hereditary set up – the human genome – and the cost of this big science project was enormous. Today, with new generation sequencing methodologies, genome sequencing has become a routine laboratory technique at relatively little cost at scale. However, it is available only in the industrialized part of the world.
At the same time, half the world’s population still lacks access to scientific progress and essential health services. Access (e.g. geographic distance and associated transport cost), availability (of qualified health workers, drugs, equipment), affordability (cost and price of services and opportunity costs) and acceptability (e.g. users’ attitudes and expectations) are important barriers to access to health services. (Jacobs et al., 2012). For example, some 800 million people spend more than 10 per cent of their household budget on health care, and almost 100 million people are pushed into extreme poverty each year because of catastrophic out-of-pocket health expenses. (WHO / World Bank Group, 2017).
The United Nations’ Sustainable Development Goals have incorporated this idea, as pointed out earlier. As Becerra-Posada points out, “Health is essential to sustainable development and is also one of its most significant achievements. Whereas only one of the 17 SDGs is exclusively about health, many others have targets or represent sectors that are essential to address the environmental and social determinants of health. As society builds sustainable cities, ends poverty and hunger while promoting equity, it also improves health. The conditions in which the world’s people are born, live, work, and age, whether they are environmental, economic, or social, determine one’s health in very profound ways, often extending beyond the health sector and health policies.” (Becerra-Posada, 2015).
Health in all policies
Meeting health needs requires input from many disciplines including the social and environmental sciences, humanities and engineering, all of which are essential for the implementation of health research. This need for interdisciplinary action extends to health policy: “Health in All Policies” is an approach to public policies across sectors that systematically takes into account the health implications of decisions, seeks synergies, and avoids harmful health impacts in order to improve population health and health equity. (Health in All Policies (HiAP) Framework for Country Action, 2014) In practice, this implies a strong programmatic and financial coordination of very different actors.
Climate change is a powerful example of how global trends (and actions to deal with them) affect health and need a Health in All Policies approach to be addressed effectively. Extreme heat causes heat stress and heat stroke, exacerbations of pre-existing heart failure, and kidney disease (The Lancet, 2017b). Natural disasters and changing rainfall patterns caused by climate change have severe implications on agriculture and nutrition, and progress made so far in tackling infectious diseases could be undermined by the effects of climate change. At the same time, many policies to reduce greenhouse-gas emissions can also have positive effects on health, e.g. reduction of air pollution, increased energy security, more sustainable mobility and transport systems. Emphasizing the positive side effects of climate mitigation measures on health may make the associated cost more acceptable to policy-makes. Likewise, policies to mitigate environmental change may have unintended adverse consequences (co-harms): Some types of biofuels, such as corn alcohol, compete directly with important food crops. Diesel engines were promoted in some countries because of their reduced greenhouse gas emissions but have higher emissions of fine particulates and nitrogen oxides. (Haines, 2017). Health should thus become an integral part of all policies, from foreign affairs, humanitarian aid and development cooperation to security, climate and environment, social and economic affairs, and research and innovation.
Collaboration across borders, policy fields and research areas is essential: The World Health Summit and the M8 Alliance
The World Health Summit is one of the world’s most prominent strategic forums for global health. The interdisciplinary event takes place within an atmosphere of academic freedom and is the premiere international platform for exploring strategic developments and decisions in the area of healthcare and setting agendas for global health. Every October, internationally renowned leaders and representatives from the sciences, politics, business, and civil society travel to Berlin for the World Health Summit to discuss the latest challenges facing medical research and healthcare. The World Health Summit, founded in 1999, enjoys the high patronage of German Chancellor Angela Merkel, the President of the French Republic Emmanuel Macron and European Commission President Jean-Claude Juncker.
The World Health Summit’s academic think tank is provided by the M8 Alliance of Academic Health Centers, Universities and National Academies, a unique collaborative network made up of leading international medical universities, research institutions and all National Academies of medicine and science. Set up under the leadership of Charité – Universitätsmedizin Berlin and along the lines of the G8 political forum, the M8 Alliance was founded on the occasion of the first World Health Summit and currently counts 25 members from 18 countries. The M8 Alliance promotes the bench to bedside strategy to population health translation of research, as well as the transformation of current medical care approaches to treating the ill by creating healthcare systems aimed at the effective prevention of disease.
At the 2017 World Health Summit, the M8 Alliance called on the countries hosting the next G7 and G20 summits and holding the presidencies of key regional organizations to include global health challenges on their agendas and to make the political choices required to ensure the implementation of the 2030 SDG agenda. Interdisciplinary collaboration is the critical factor – all stakeholders from academia, the private sector, civil society and politics have to work together. Governments have to coordinate their activities, support international cooperation and strengthen the World Health Organization (WHO). The Sustainable Development Goals have provided the road map for action.” They emphasized that “The world needs strong global health institutions to set norms and standards, respond to outbreaks and to protect and support the most vulnerable”. (M8 Alliance, 2017).
The World Health Summit has thus become a unique forum to garner high-level political, academic and industry support for global health. As stakeholders from areas other than health contribute to World Health Summit, health actors need to ensure their participation at other fora such as the Munich Security Conference, or the Global Solutions Summit to ensure global health is represented in all political dialogues and ultimately in all policies. Such transdisciplinary, cross-sectoral concerted efforts are necessary to set the agenda for global health and to ultimately improve health and wellbeing globally.
References
- Beaglehole, R., & Yach, D. (2003). Globalisation and the prevention and control of non-communicable disease: The neglected chronic diseases of adults. The Lancet, 362(9387), 903-908. doi:10.1016/s0140-6736(03)14335-8
- Bloom, D.E., Cafiero, E.T., Jané-Llopis, E., Abrahams-Gessel, S., Bloom, L.R., Fathima, S., Feigl, A.B., Gaziano, T., Mowafi, M., Pandya, A., Prettner, K., Rosenberg, L., Seligman, B., Stein, A., & Weinstein, C. (2011). The Global Economic Burden of Non-communicable Diseases. Geneva: World Economic Forum. Retrieved April 27, 2018 from https://apps.who.int/medicinedocs/documents/s18806en/s18806en.pdf
- Chopra M, Galbraith S, Darnton-Hill I. (2002): A global response to a global problem: the epidemic of overnutrition. Bull World Health Organ (2002) 80(12):952–8
- Deloitte (2016). 2017 Global Life Sciences Outlook. Retrieved April 24, 2018, from https://www2.deloitte.com/content/dam/Deloitte/global/Documents/Life-Sciences-Health-Care/gx-lshc-2017-life-sciences-outlook.pdf
- Dye, C., & Acharya, S. (2017). How can the sustainable development goals improve global health? A call for papers. Bulletin of the World Health Organization, 95(10). doi:10.2471/blt.17.202358
- Ganten, D., & Nesse, R. (2012). The evolution of evolutionary molecular medicine. Journal of Molecular Medicine, 90(5), 467-470. doi:10.1007/s00109-012-0903-2
- Glover, M., Buxton, M., Guthrie, S., Hanney, S., Pollitt, A., & Grant, J. (2014). Estimating the returns to UK publicly funded cancer-related research in terms of the net value of improved health outcomes. BMC Medicine, 12(1). doi:10.1186/1741-7015-12-99
- Glover, M., Montague, E., Pollitt, A., Guthrie, S., Hanney, S., Buxton, M., & Grant, J. (2018). Estimating the returns to United Kingdom publicly funded musculoskeletal disease research in terms of net value of improved health outcomes. Health Research Policy and Systems, 16(1). doi:10.1186/s12961-017-0276-7
- Haines, A. (2017). Health co-benefits of climate action. The Lancet Planetary Health, 1(1). doi:10.1016/s2542-5196(17)30003-7
- Health in All Policies (HiAP) Framework for Country Action. (2014). Health Promotion International, 29(Suppl 1), I19-I28. doi:10.1093/heapro/dau035
- Ipsos Public Affairs (2017): What Worries the World. Retrieved April 24, 2018, from https://www.ipsos.com/sites/default/files/2017-08/What_worries_the_world-July-2017.pdf
- Jacobs, B., Ir, P., Bigdeli, M., Annear, P. L., & Damme, W. V. (2011). Addressing access barriers to health services: An analytical framework for selecting appropriate interventions in low-income Asian countries. Health Policy and Planning, 27(4), 288-300. doi:10.1093/heapol/czr038
- M8 Alliance (2017). M8 Alliance Declaration. World Health Summit 2017. Health is a political choice. Retrieved April 24, 2018, from: https://d1wjxwc5zmlmv4.cloudfront.net/fileadmin/user_upload/downloads/2017/WHS_Berlin/Data/M8_Alliance_Declaration_2017_Berlin.pdf
- Sobocki, P., Lekander, I., Berwick, S., Olesen, J., & Jönsson, B. (2006). Resource allocation to brain research in Europe (RABRE). European Journal of Neuroscience, 24(10), 2691-2693. doi:10.1111/j.1460-9568.2006.05116.x
- Steyn K, Damasceno, A. (2006). Lifestyle and Related Risk Factors for Chronic Diseases. In Jamison, D. T. (2006). Disease and mortality in Sub-Saharan Africa. Washington, D.C.: World Bank. Retrieved April 24, 2018, from https://www.ncbi.nlm.nih.gov/books/NBK2290/
- The Lancet (2017a). Life, death, and disability in 2016. The Lancet, 390(10100), 1083.
- The Lancet (2017b). Climate change and health. Retrieved April 24, 2018, from https://www.thelancet.com/infographics/climate-and-health
- United Nations (2017). 2017 Revision of World Population Prospects. Retrieved 04 24, 2018, from https://esa.un.org/unpd/wpp/Publications/Files/WPP2017_KeyFindings.pdf
- United Nations (1999). The World at Six Billion. Retrieved April 24, 2018, from Department of Economic and Social Affairs: https://www.un.org/esa/population/publications/sixbillion/sixbillion.htm
- WHO / World Bank Group. (2017, December). Tracking universal health coverage: 2017 Global Monitoring Report. Retrieved April 24, 2018, from https://www.who.int/healthinfo/universal_health_coverage/report/2017/en/
- WHO (2017). Noncommunicable diseases. Retrieved April 24, 2018, from https://www.who.int/en/news-room/fact-sheets/detail/noncommunicable-diseases
- Wooding, S. (2011). Project Retrosight: Understanding the returns from cardiovascular and stroke research: The Policy Report. Retrieved April 24, 2018, from RAND Corporation: https://www.rand.org/pubs/monographs/MG1079.html.