There is an urgent need for collective action to improve key aspects of our global health that can be realized only by addressing the global systemic and structural health inequities that impose significant social, economic, and inter-generational costs. Health disparities have continued to increase within and across countries, regions, and continents, despite gains in some localities. COVID-19 has amplified health inequities that disproportionately impact poor and vulnerable groups around the world. The global scramble to respond to the COVID-19 pandemic has demonstrated the need for a global reaffirmation of health as being integral to the social, economic, and environmental resilience of our planet. Equitable approaches to COVID-19 and future shocks require global collective action on Global Public Goods for health.[1]
Challenge
Global health inequities have continued to increase within and across countries, regions, and continents, with gains seen in some areas. Economic shocks, social upheavals, natural disasters, and public health emergencies exacerbate and widen these inequities. The COVID-19 pandemic is one example of such emergencies. It has amplified the systemic and structural inequities, including health inequities, that disproportionately and negatively impact poor and under-represented groups across and within communities, countries, regions, and continents. The challenge and ongoing discourse about the response to COVID-19, its prevention and treatment, and the development and fair global allocation and distribution of COVID-19 vaccines hinges on effective collaboration between nations and a strong commitment to ensuring that the most vulnerable populations are protected and vaccinated. The poor and marginalized are bearing the brunt of the health and economic impacts of COVID-19; yet, they may be the last in line to receive new diagnostics, treatments, and vaccines when they become available.
The implementation and adherence to prevention guidelines and strategies has been a challenge in the Global North as well as in the Global South, and more so in the Global South, where there is a preponderance of fragile and conflict-affected states (FCS) and forced displacement of population groups – 79.5 million worldwide at the end of 2019.[2] In FCS, the total expenditure on health as a percentage of GDP is significantly low – 6.98% compared to 9.94% globally.[3] Furthermore, an estimated one billion people live in urban slums or informal settlements and are highly susceptible to COVID-19 infection (Lilford et al 2016; Snyder, Marlow and Riley 2017[4]) Equitable approaches to the COVID-19 response and future shocks must recognize these realities.
Immediate government responses to the COVID-19 pandemic cover a wide spectrum: denial; closing borders; commandeering personal protective equipment (PPE); competing for priority access to or ownership of emerging diagnostics, therapies, and vaccines; crowd-sourcing therapies and vaccines; and raising funds for a global response and support of multilateral organizations to respond. This spectrum represents an evolution of responses by some leaders from trying to attack the pandemic independently to pivoting and re-focusing on a collective response. This collective response must be celebrated and strengthened, since preventive measures to contain the transnational spread of COVID-19 and future diseases are only as effective as those in the country exercising the least care. There must be a recognition that in “… the twenty-first century, disease events are no longer exclusive domestic concerns of national authorities” (Aginam 2001).
Proposal
This Policy Brief considers Global Public Goods (GPGs) for health as being essential to address the systemic and structural health inequities that impose significant social, economic, and inter-generational costs globally, even as the wealth gap continues to increase. This consideration is presented to reaffirm the need for global collective action in global health security, health system strengthening, research and development for health, and disease prevention, transmission, and control, including vaccine coverage. The essence of the GPG concept is that the argument for self-protection and self-preservation is inexorably bound up with a recognition of mutual vulnerabilities. The transcendent “self” cannot be protected or preserved without recognition of interdependence. As noted by Acharya (2020), “The real argument of interdependence theory is not that it prevents conflict, but that it makes conflict more costly to all parties in an interdependent relationship. The coronavirus has proven just that.” We must think beyond the boundaries of individual nation states and see health as transnational. We face transnational health risks and need collective action to prevent, control, and mitigate them.
The global scramble to respond to the COVID-19 pandemic has reaffirmed the need for a global reset on the role of health in the social, economic, and environmental resilience of our planet. Smith (2003), Smith et al. (2003) and Smith and MacKellar (2007) have long asserted that the notion of a global public good (GPG) “can be a powerful tool in promoting global health because it marshals arguments of self-interest. It can be used to identify areas in which global collective action is needed, specify where the costs and benefits will rest and communicate to the public why spending to promote health thousands of kilometers around the world is not a waste of their tax dollars.” (Smith et al. 2003).
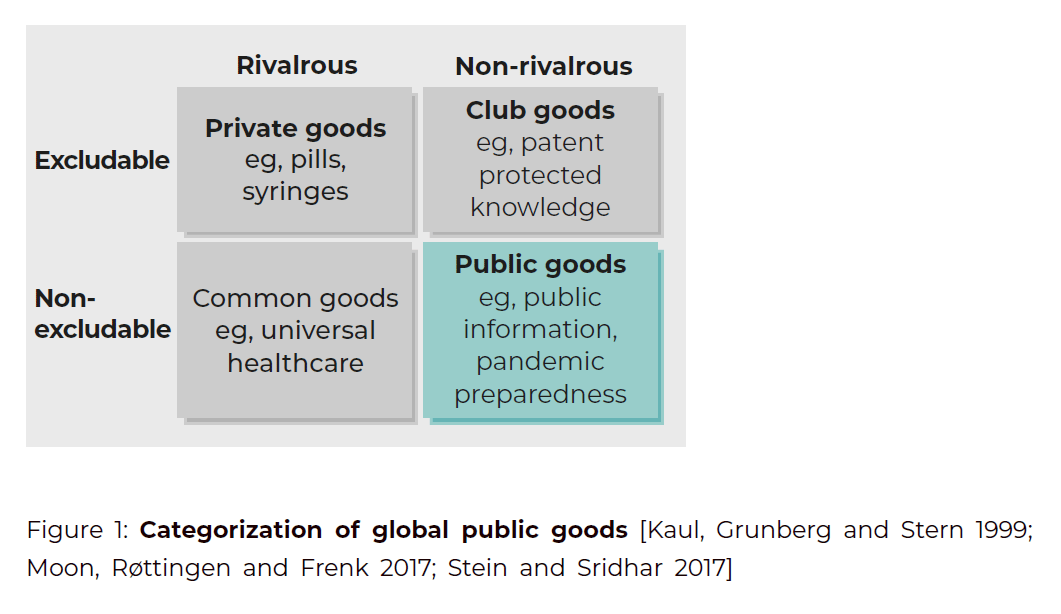
Conceptually, global public goods describe any material or immaterial entity according to whether it is excludable (i.e., can a party be stopped from consuming it?) or rivalrous (i.e., does its consumption reduce its availability for others?). Depending on these two features, scholars divide entities into four types: private goods (e.g., pills and syringes), club goods (e.g., knowledge protected by patent), common goods (e.g., universal healthcare), and public goods (e.g., public information or pandemic preparedness). Pure public goods are usually entities that are non-rivalrous and non-excludable (Moon, Røttingen and Frenk 2017; Stein and Sridhar 2017)
Galea (2016), drawing on the lessons of the Ebola and SARS epidemics, observed that “notions of nation-specific public goods are quaint and that the provision of public health is dependent on global public goods that may require universal solutions.” The emergence of COVID-19, and its unfolding economic, social, and political impacts across the globe, has catapulted the GPG for health issue to the forefront. Broad policy failures and breakdowns in supply chains as governments scramble to frame policy responses and mobilize resources in the face of the rapidly spreading pandemic have been compounded by rising human costs in terms of mortality and the related economic and social costs. It is increasingly evident that we must develop and adopt a robust national and a global view of health as a public good.
While economists may use the term GPGs in a narrow sense to refer specifically to non-rival, non-excludable goods, the global health community has started using the term more broadly. For example, the WHO refers to “common goods for health (CGH),” which include GPGs for health and goods and services with large social externalities (Soucat 2019). These common goods for health fall into five categories: policy and coordination, taxes and subsidies, regulation and legislation, information, analysis and communication, and population services. The Lancet Commission on Investing Health (the CIH) proposed the term “global functions” to refer to “activities that go beyond the boundaries of individual nations to address transnational issues” (Yamey et al 2019). The CIH recognizes three types of global functions: GPGs for health (e.g., product development for neglected or emerging infectious diseases); managing regional or global negative externalities (e.g., pandemic preparedness, tackling antimicrobial resistance); and fostering leadership and stewardship (e.g., strengthening the WHO’s core functions) (Jamison et al 2013). These functions, argued the CIH, have been critically neglected and under-funded. The interlinkages between these categorizations are self-evident. More importantly, however, it is apparent that the G20 has a critical role in the policy, institutional, and scientific actions required at every level.
More difficult global health challenges such as the COVID-19 pandemic require the contribution and actions of many sectors and systemic interventions to support the provision of GPGs for health (Kickbusch and Reddy 2015). Evidence suggests that there is an increased need for investments in GPGs for health. The CIH found that, in 2013, only about one-fifth of all donor financing was directed towards global functions (Schäferhoff et al 2015). In a follow-up study, they found that the proportion rose after the 2014-2016 Ebola epidemic in West Africa, but then fell again once the epidemic was under control, showing the reactive (rather than proactive) nature of external funding for global functions. Increased investments to support interventions towards achieving GPGs for health and greater multilateral cooperation on GPGs are warranted now more than ever in response to the COVID-19 pandemic and to prepare for future threats. It is encouraging that even before the COVID-19 pandemic, the four main multilateral health funders (the World Bank, the Global Fund to Fight AIDS, Tuberculosis and Malaria, Gavi, the Vaccine Alliance, and the WHO) envisioned three ways to strengthen their multilateral cooperation on GPGs for health (Yamey et al 2018):
- Improving the production, quality and use of health data
- Accelerating the development and access to health technologies in low- and middle-income countries
- Strengthening global health security, particularly epidemic and pandemic preparedness.
This need is even greater in the Global South where systemic global disparities and inequities place more than half of the world’s population at great health risk. Moreover, it behooves the developed economies to take action on GPGs for health since their very survival rests on it. The COVID-19 pandemic has not only debunked their invincibility and exposed their mutual vulnerabilities, as the “… fact that the political boundaries of sovereign states do not represent natural barriers to infectious agents …. underscores the need for interstate cooperation to address these global health issues.” (Aginam 2001). The United Nations Secretary General, António Guterres, is constant in his request to the world community and our leaders be unified in our response: “Unless we act now, the COVID-19 pandemic will cause unimaginable devastation and suffering around the world … We need to respond with unity and solidarity” (2020).
A. Recommendations
In the face of current global challenges and disruptions occasioned by the COVID-19 pandemic, we have to act together and build on the strength and global reach of our multilateral institutions. Whether we speak of GPG or common goods for health, it is imperative that there be global collective action. The current COVID-19 pandemic acutely highlights that this and any other emerging infectious disease with pandemic potential must be tackled with global collection action. Until every country is disease free, no country will be disease free. What the world needs now more than ever is a global health body emboldened, supported, and fully financed. We must recall that, historically, the WHO has played a central role in providing a broad range of GPGs for health (Moon, Røttingen and Frenk 2017).
However, the inherent funding challenges of the WHO often paralyze its ability to be the global coordinating body for health, and prepared and respond to the pandemics. After the Ebola outbreak, in 2015, the World Health Assembly established the Contingency Fund for Emergencies (CFE) that finances WHO Health Emergency Programme to respond to the pandemics, but the CFE is yet to obtain adequate resources (Reddy, Mazhar and Lencucha 2018).
The way in which the WHO is funded is also impeding the provision of GPGs for health. WHO is funded in two ways: through the dues that member states pay (these are scaled by income and population) and through “voluntary contributions” (also called extra-budgetary funds) from a small number of donors. Over the last two decades, there has been a major shift in the distribution of WHO’s income between these two types. In WHO’s 1994-95 budget, voluntary contributions comprised 40% of all funding, but they rose steadily and reached almost 80% in the 2018-19 budget (Yamey et al 2019). Why should this trend cause alarm? Because voluntary contributions are heavily earmarked—that is, the donors tell WHO what to spend the funding on (e.g., polio eradication). These extra-budgetary funds do not finance the WHO’s core responsibilities in provision of GPGs. The CIH argues that, as a result of earmarking by donors, WHO is “struggling to fund its core functions, undermining its capacity to supply global public goods and other global functions, including the management of negative externalities.” (Watkins et al 2018).
While we ensure full funding of the WHO’s core functions as the existing global coordinating body for global health, we also need multilateral economic and political institutions such as the World Bank, the International Monetary Fund (IMF), the Organization for Economic Cooperation and Development (OECD), and the European Union (EU) to come together in unprecedented ways to work with the WHO and link, once and for all, health with economics for COVID-19 response. Led by Kristalina Georgieva, the IMF recognizing that these are dangerously unprecedented times, “has doubled access to its emergency facilities, approved debt service relief for 25 low-income countries through a reformed Catastrophe Containment and Relief Trust (CCRT) ….” For Georgieva, “the global coronavirus outbreak is a crisis like no other and poses daunting challenges for policymakers in many emerging market and developing economies (EMDEs), especially where the pandemic encounters weak public health systems, capacity constraints, and limited policy space to mitigate the outbreak’s repercussions.”
B. The G20’s Role in Reaffirming the Importance of Global Public Goods for Health – Call to Action and Recommendations
Building on the foundation of the G20’s leadership role in managing the global financial crisis and coordinating with the Bretton Woods institutions mandated to take action, the G20 was effective in building consensus, mobilizing resources, leveraging its collective political weight, and taking action. As noted by Luckhurst et al (2020), the G20 is capable of implementing a transversal policy strategy and is “suited to providing strategic leadership, making recommendations for and supporting cooperation across its policy agenda on issues also covered within the mandate of the existing global institutions.”
Global health challenges, such as reducing global health inequalities or ensuring global health security, cannot be achieved by a single organization or through sovereign institutions such as ministries of health. It requires the strategic link with other transnational agendas and a strengthening of the political ability to position health interests (Kickbush and Reddy 2015). The G20 should play a leadership role in reforming, strengthening, and operationalizing the global governance framework for health as a global public good. The G20 must facilitate the integration of health in transnational political and global governance agendas.
Global public goods for health include programs, policies, and services that have a transnational reach and there is an urgent need to establish independent mechanisms to coordinate decision-making on health security. There is increased support among global leaders for framing the COVID-19 vaccines as a GPG; thus, the G20 should recognize COVID-19 vaccines as a GPG.[5] We ask the G20 to strategize independent mechanisms to address the transborder spread of pathogens, ensure global health security, and promote Global Solidarity in Response to COVID-19 and Future Shocks. The G20 must take collective action to promote the health of every human being, especially the most vulnerable, by recognizing our mutual vulnerabilities and transnational health risks.
In this, the last decade for realizing the Sustainable Development Goals (SDGs), the SDGs offer “a unique opportunity to address the social, economic and political determinants of health and improve the health and wellbeing of people everywhere” (WHO 2020) Specifically, we recommend that the G20 take immediate steps to:
- Reaffirm the commitment to universal health coverage (UHC) as a means to improving health outcomes and reducing health disparities.
- Invest in research and development capacity building, including adequate funding, in LMICs.
- Ensure supply and access to COVID-19 therapeutics and diagnostics, in addition to vaccines, in the Global South.
- Place health at the center of people-centric economic and social strategies and their implementation: It is essential to integrate access to health care and protection from infectious disease outbreaks into the world’s security, economic, and development agendas.
- Reform, strengthen, and operationalize a robust and effective global governance framework for health: It is essential to strengthen the existing multilateral organizations[6] mandated to carry out critical functions within this framework. In addition, safeguards must be put in place to ensure the integrity, transparency, and accountability of the bodies within the framework.
- Commit to funding and supporting Resilience and Preparedness globally.
- Ensure equitable access to vaccines, therapeutics, and diagnostics, and minimize access gaps between the Global North and the Global South.
- Build consensus, commit to action, and take action on special-purpose vehicles to lead and effect global changes in health, public health, and health systems.
Urgent action on these recommendations is essential for global solidarity and a sustainable collective response to the COVID-19 pandemic and future shocks.
Acknowledgement
The lead author wishes to acknowledge the substantive contributions of Osondu Ogbuoji, Duke Global Health Institute, Duke University; K. Srikanth Reddy, Bruyère Research Institute; Margo Thomas, Women’s Economic Imperative; and Gavin Yamey, Duke Global Health Institute, Duke University
Disclaimer
This policy brief was developed and written by the authors and has undergone a peer review process. The views and opinions expressed in this policy brief are those of the authors and do not necessarily reflect the official policy or position of the authors’ organizations or the T20 Secretariat.
References
Acharya, A. 2020. “How Coronavirus May Reshape the World Order.” The National
Interest, article, April 18, 2020. https://nationalinterest.org/feature/how-coronavirus-may-reshape-world-order-145972.
Aginam, Obijiofor. 2001. “From Isolationism to Mutual Vulnerability and Back: International
Law and Unfair Distribution of Global Disease Burdens.” In Proceedings of
the ASIL Annual Meeting. 95: 58-64. https://doi.org/10.1017/S0272503700056615.
Galea, Sandro. 2016. “Public Health as a Public Good.” Dean’s Note. BU School of Public
Health, January 10, https://www.bu.edu/sph/2016/01/10/public-health-as-a-publicgood.
Guterres, António. 2020. “Opening Remarks at Joint Press Conference on the
High-Level Event on Financing for Development in the Era of COVID-19 and Beyond.”
United Nations, May 28, 2020. https://www.un.org/sg/en/content/sg/speeches/
2020-05-28/remarks-press-conference-financing-for-development-era-of-covid-19-and-beyond.
Jamison, Dean T., Lawrence H. Summers, George Alleyne, Kenneth J. Arrow, Seth
Berkley, Agnes Binagwaho, Flavia Bustreo et al. 2013. “Global Health 2035: A World
Converging Within a Generation.” The Lancet 382, no. 9908: 1898-955. https://doi.org/10.1016/S0140-6736(13)62105-4.
Kickbusch, Ilona S. and K. Srikanth Reddy. 2015. “Global Health Governance – The
Next Political Revolution.” Public Health 129, no. 7: 838-42. https://doi.org/10.1016/j.puhe.2015.04.014.
Kaul, Inge, Isabelle Grunberg, and Marc Stern. 1999. “Defining Global Public Goods.”
In Global Public Goods: International Cooperation in the 21st Century, edited by Inge
Kaul, Isabelle Grunberg, and Marc Stern, 2–19. Oxford: Oxford University Press. https://doi.org/10.1093/0195130529.003.0001.
Lilford, Richard J., Oyinola Oyebode, David Satterthwaite, G. J. Melendez-Torres, Yen-
Fu Chen, Blessing Mberu, Samuel I. Watson et al. 2016. “Improving the Health and
Welfare of People Who Live in Slums.” The Lancet 389, no. 10068: 559–70. https://doi.org/10.1016/S0140-6736(16)31848-7.
Luckhurst J, Thomas M, Kirton J, Fleurbaey M, Grimalda, G, Sidiropoulos E, Ertl V,
Knight WA, Reddy, KS. 2020 (Forthcoming). Transversal G20 response to COVID-19:
Global governance for economic, social, health, and environmental resilience. Task
Force 11: (COVID-19) Multidisciplinary Approaches to Complex Problems.
Moon, Suerie, John-Arne Røttingen, and Julio Frenk. 2017. “Global Public Goods for
Health: Weaknesses and Opportunities in the Global Health System.” Health Economics,
Policy and Law 12, no. 2: 195–205. https://doi.org/10.1017/S1744133116000451.
Reddy, Srikanth K., Sumaira Mazhar, and Raphael Lencucha. 2018. “The Financial
Sustainability of the World Health Organization and the Political Economy of Global
Health Governance: A Review of Funding Proposals.” Globalization and Health 14, no.
119. https://doi.org/10.1186/s12992-018-0436-8.
Schäferhoff, Marco, Sara Fewer, Jessica Kraus, Emil Richter, Lawrence H. Summers,
Jesper Sunderwall, Gavin Yamey, and Dean T. Jamison. 2015. “How Much Donor Financing
for Health is Channeled to Global Versus Country-Specific Functions?” The
Lancet 386, no. 10011: 2436–41. https://doi.org/10.1016/S0140-6736(15)61161-8.
Smith, Richard D. 2003. “Global Public Goods and Health.” Bulletin of the World
Health Organization, 81, no. 7: 475.
Smith, Richard, Robert Beaglehole, David Woodward, and Nick Drager (Eds.) 2003.
Global Public Goods for Health: Health Economic and Public Health Perspectives.
Oxford: Oxford University Press.
Smith, Richard D. and Landis MacKellar. 2007. “Global Public Goods and the Global
Health Agenda: Problems, Priorities and Potential.” Globalization and Health 3, no. 9.
https://doi.org/10.1186/1744-8603-3–9.
Snyder, Robert E., Mariel A. Marlow, and Lee W. Riley. 2014. “Ebola in Urban Slums:
The Elephant in the Room.” The Lancet Global Health 2, no. 12: e685. https://doi.org/10.1016/S2214-109X(14)70339-0.10.
Soucat, Agnès. 2019. “Financing Common Goods for Health: Fundamental for Health,
the Foundation for UHC.” Health Systems & Reform 5, no. 4: 263–67. https://doi.org/10.1080/23288604.2019.1671125.
Stein, Felix and Devi Sridhar. 2017. “Health as a ‘Global Public Good’: Creating a Market
for Pandemic Risk.” BMJ 358: j3397. https://dx.doi.org/10.1136/bmj.j3397.
Watkins, David A., Gavin Yamey, Marco Schäferhoff, Olusoji Adeyi, George Alleyne,
Ala Alwan, Seth Berkley et al. 2018. “Alma-Ata at 40 Years: Reflections from the Lancet
Commission on Investing in Health.” Lancet 392, no 10156: 1434–60. https://doi.org/10.1016/S0140-6736(18)32389-4.
World Health Organization. 2020. Director-General Vision Statement. Accessed August
27, 2020. https://www.who.int/dg/vision.
World Health Organization. 2020. “Strategic Preparedness and Response Plan.”
World Health Organization, Infographic. Last updated August 14, 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/strategies-plans-and-operations.
Yamey, Gavin, Kaci Kennedy, Jessica Kraus, Hugo Petitjean, Christina Schrade, Sara
Fewer, Naomi Beyeler and Nina Schwalbe. 2018. Intensified Multilateral Cooperation
on Global Public Goods for Health: Three Opportunities for Collective Action. Policy
Paper. Durham (NC): Center for Policy Impact in Global Health.
Yamey, Gavin, Dean Jamison, Odd Hanssen, and Agnès Soucat. 2019. “Financing
Global Common Goods for Health: When the World is a Country.” Health Systems &
Reform 5, no. 4: 334–49. https://doi.org/10.1080/23288604.2019.1663118.
Appendix
[1] . The use of the term Global Public Good recognizes the fact that key aspects of our global health require the need for international collective action: health security; research and development; disease transmission and control; vaccine development and coverage.
[2] . UNHCR Global Trends, Forced Displacement in 2019. Key health indicators such as life expectancy (the average life expectancy in FCS is 62.2 years, 9 years lower than the global average of 71.4 years; under five and maternal mortality; health service coverage, including vaccine accessibility; and the burden of disease – infectious and non-communicable add to these issues.
[3] . The anticipated economic shocks and responses to COVID-19 by high-income countries (HICs) could lead to lower DAH over the next few years which would affect low-income countries (LICs) the most.
[4] . The lack of or near absence of basic necessities such as water, soap, toilets, sewers, drainage, waste collection, and secure and adequate housing are compounded by violence, overcrowding, and pre-existing comorbidities making physical distancing and self-quarantine impractical.
[5] . The Agreement on Trade-Related Aspects of Intellectual Property Rights (TRIPS) sets minimum standards for intellectual property (IP) protection for World Trade Organization (WTO) Member States. In 2001, in the Doha declaration on TRIPS and Public Health adopted by the Ministerial Conference of the WTO affirmed that governments could override patents in public health emergencies. Based on this, a tiered pricing system was developed in which drug companies make profits in richer countries while allowing medicines to be sold more cheaply in poorer ones.
[6] . This constellation of actors includes the WHO, the World Bank, and the International Monetary Fund (IMF). For example, while strengthening the WHO with increased resources, there is an urgent need to develop accountability framework (s) for the International Health Regulations (IHR) compliance.